
Corns and calluses are common skin conditions caused by repeated friction or pressure on specific areas of the skin. They typically form on the feet and hands as a protective response to prevent further irritation.
Corns often develop on the tops and sides of toes, or on the sole of the foot, as a result of ill-fitting shoes, abnormal gait, or deformities like hammertoe. Calluses, on the other hand, typically form on the palms, fingers, or soles of the feet due to repetitive actions or pressure.
To prevent the recurrence of corns and calluses, it’s essential to continue wearing well-fitting shoes, using orthotics if recommended, and maintaining good foot hygiene.
Livingstone Dermatology provides comprehensive care for corns and calluses. Our experienced dermatologist will assess your condition and recommend a personalized treatment plan to alleviate discomfort and help you achieve healthy, pain-free skin.
Cysts and abscesses are common skin conditions characterized by the formation of enclosed pockets of fluid, pus, or other materials within or beneath the skin. While they may appear similar, they have distinct characteristics and treatment approaches.
Cysts are closed sacs filled with fluid, semi-solid material, or air. They can develop anywhere on the body and vary in size. Cysts are typically non-cancerous and can be caused by a variety of factors, including infection, blockage of ducts, or genetic predisposition.
Abscesses, on the other hand, are localized infections that result in the accumulation of pus. They often occur in response to bacterial infections, usually as a result of a wound or hair follicle infection. Abscesses are characterized by redness, swelling, pain, and often have a visible “head” or opening.
Proper wound care, maintaining good hygiene, and seeking prompt treatment for any skin infections can help prevent the recurrence of cysts and abscesses.
Livingstone Dermatology offers specialized care for cysts and abscesses. Our experienced dermatologist will assess your condition and recommend a personalized treatment plan to promote healing and prevent future occurrences.
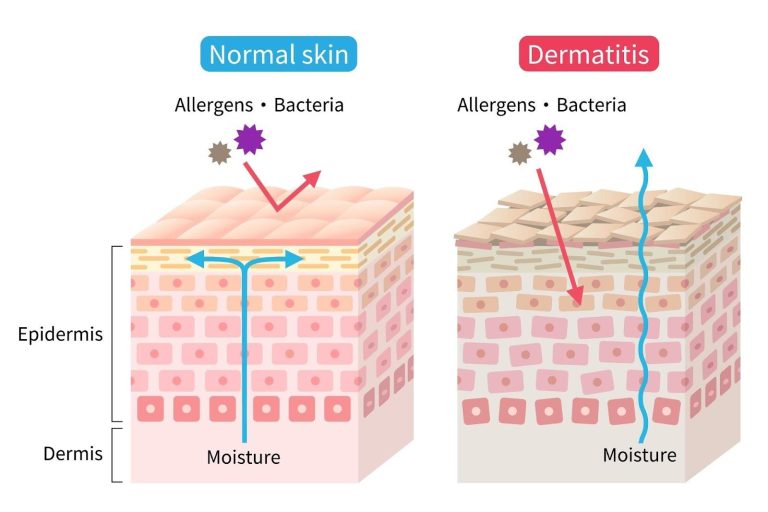
Eczema, also known as dermatitis, is a common skin condition characterized by red, itchy, and inflamed skin. It often appears in patches and can range from mild to severe. Livingstone Dermatology is here to provide comprehensive care and relief for individuals dealing with eczema.
Eczema is a chronic skin condition that results from a combination of genetic and environmental factors. It is characterized by inflammation of the skin’s outer layer, leading to symptoms such as redness, itching, and the development of dry, scaly patches.
While the exact cause of eczema is not fully understood, it is believed to be related to a combination of factors, including genetics, an overactive immune response, and environmental triggers like allergens or irritants.
In addition to medical treatments, adopting a consistent skincare routine and avoiding known triggers can significantly improve the management of eczema.
At Livingstone Dermatology, our experienced dermatologist is dedicated to providing personalized care for individuals with eczema. We work closely with each patient to develop a customized treatment plan aimed at providing relief and improving the overall health of the skin.

Sweating is a normal bodily function that helps regulate temperature. However, for some individuals, excessive sweating occurs regardless of temperature or physical activity. This condition, known as hyperhidrosis, affects daily life, causing discomfort, and social anxiety. Fortunately, various treatments are available to help manage excessive sweating effectively.
Hyperhidrosis is a medical condition characterised by excessive sweating that goes beyond what is necessary for temperature regulation. It can affect different parts of the body, including the palms, soles, underarms, and face. This condition is typically caused by overactive sweat glands, leading to persistent sweating – even when at rest.
Hyperhidrosis is categorised into two main types, which are:
The overstimulation of the sweat glands, due to the influence of the nervous system, is typically the cause of hyperhidrosis. Be that as it may, the causes can be divided into two categories:

Some of the common symptoms of hyperhidrosis are:
Beyond physical discomfort, hyperhidrosis can significantly impact daily life, and mental well-being:
The eccrine glands are responsible for producing sweat. As it exists in the skin throughout the body, symptoms of hyperhidrosis can occur anywhere, with the following areas being the primary areas:
When it comes to hyperhidrosis, it is important to manage the triggers. There are certain factors that can worsen hyperhidrosis episodes, including:

Diagnosing hyperhidrosis involves a thorough evaluation to determine the type, severity, and potential underlying causes of excessive sweating. At Livingstone Dermatology, our dermatologists begin with a detailed consultation, and physical examination.
During the initial consultation, our dermatologists will assess your symptoms through:
In addition to a physical examination, our dermatologists may recommend specific tests to confirm the diagnosis, and assess the severity of the condition:
Treatment for hyperhidrosis is primarily focused on managing the condition, and preventing it from exacerbating. As such, it includes a variety of treatment options, ranging from conservative measures to more invasive forms of medical intervention – all of which are tailored specifically to each patient.
For mild to moderate hyperhidrosis, conservative methods can help manage excessive sweating:

For moderate to severe hyperhidrosis, medical treatments offer longer-lasting relief:
For severe hyperhidrosis that does not respond to other treatments, surgical interventions may be considered:
Excessive sweating can be disruptive, and challenging to manage on your own. Thankfully, there are several medical-grade treatments that can help you manage hyperhidrosis symptoms effectively.
Schedule a consultation today for a detailed diagnosis and personalised treatment plan.
Normal sweating occurs as a natural response to heat, physical activity or emotional stress, helping to regulate body temperature. It usually stops once the triggering factor subsides.
Excessive sweating, on the other hand, happens regardless of external conditions, and can interfere with daily activities. The key differences include:
Hyperhidrosis affects approximately 2 – 3% of the global population, with many cases remaining undiagnosed or untreated. This is largely due to a lack of awareness, and education related to the condition.
Most people with hyperhidrosis do not experience body odour. However, to prevent body odour (bromhidrosis), you can:
There is no conclusive evidence linking regular use of these products to breast cancer. Many formulations, including natural and clinical-strength options, are available, allowing individuals to choose what suits them best.
It is important to seek medical attention for hyperhidrosis to prevent the following potential complications:
Although treatment-related side effects are uncommon, it is important to be aware of the potential side effects. These side effects depend on the treatment method, but may include:
It is important to understand that most treatments provide temporary relief. As such, it requires repeated sessions or long-term management. However, surgical options may offer a permanent solution, but they do come with their own set of risks.
While hyperhidrosis itself may not be preventable, triggers can be managed through lifestyle adjustments, appropriate treatments.
Yes, some lifestyle adjustments can help. This includes:
Living with hyperhidrosis can be challenging, but effective treatment options are available. Our experienced dermatologist will work with you to develop a personalized treatment plan that addresses your specific concerns and provides lasting relief.

Scars are our body’s way of protecting us after the skin is injured. When the dermis is damaged, our body produces collagen fibres to repair the wound. This is laid down rapidly and densely, creating a scar.
However, when excess collagen is produced during the healing process, keloid scars can form. These are raised scars that form beyond the original wound — thick, raised, and sometimes, darker than the surrounding skin. While they do not pose serious health risks, their appearance, and potential discomfort can be distressing. Fortunately, various treatments are available to help reduce, and manage keloid scars, restoring both skin appearance and self-assurance.
Keloid scars are an overgrowth of scar tissue that forms at the site of a skin injury. Unlike regular scars, keloids extend beyond the original wound, and may continue to grow over time. This occurs due to excessive collagen production during the healing process. Instead of gradually fading, keloid scars become thick, raised, and sometimes itchy or uncomfortable. They can develop after minor skin injuries such as cuts, burns, acne or even piercings. Although harmless, their noticeable appearance can be a cosmetic concern for many individuals.
Identifying, and differentiating keloid scars is essential for seeking the right treatment. In fact, understanding their unique characteristics can help individuals determine the most ideal course of action.
Keloids can appear anywhere on the body but are more common in areas with high skin tension, and movement, including:
Keloid scars have distinct visual, and physical characteristics, such as:
Keloids form when the body produces excessive collagen while healing an injury. Collagen is a structural protein that helps repair, and strengthen the skin. However, in some individuals, an overproduction of collagen leads to the formation of keloid scars. Unfortunately, the exact reason behind this excessive collagen production remains unclear.
Keloids may develop after various skin injuries or conditions, including:

In addition to medical treatments, adopting a consistent skincare routine and avoiding known triggers can significantly improve the management of eczema.
The symptoms of keloid scars can vary but often include:
Although anyone can have keloid scars, there are certain individuals that are more prone to developing keloid scars due to genetic, and environmental factors. The risk factors include:
Several methods for assessing keloid scars include:

Treatment for keloid scars is tailored based on the severity, size, and location of the scar. At Livingstone Dermatology, our dermatologists may recommend one or a combination of the following treatment options:
While keloid scars can be persistent, and impact self-confidence, they are manageable with the right treatment approach. It is important to remember that early intervention is key to preventing excessive scar growth. At Livingstone Dermatology, we offer comprehensive keloid scar assessments, and medical-grade treatment options to help you achieve smoother, healthier skin. Contact us today for a personalised treatment plan.
Keloids are often mistaken for hypertrophic scars, a more common type of scarring. Hypertrophic scars are typically flat and vary in colour from pink to brown. They are smaller than keloids and, unlike keloids, may gradually fade over time.
Both men and women experience hypertrophic scars at similar rates, and they can affect individuals of all skin tones. These scars often result from physical or chemical injuries, such as piercings or exposure to harsh substances. Initially, hypertrophic scars may be itchy or painful, but these symptoms generally lessen as the skin heals.
Keloid scars are not always painful, but some people may experience discomfort, tenderness or itching in the affected area. The severity of symptoms varies from person to person, and larger keloids may cause more noticeable discomfort.
If pain or irritation is affecting your daily life, treatment options are available to help relieve symptoms and improve the appearance of the scar.
While keloid scars are not harmful to your overall health, they can sometimes lead to discomfort, restricted movement (if they develop over joints) or emotional distress due to their appearance. Additionally, keloids can sometimes continue to grow over time.
Most keloid treatments involve minimal downtime. Procedures like corticosteroid injections, laser therapy, and cryotherapy allow patients to resume normal activities almost immediately. However, surgical removal or radiation therapy may require a brief recovery period.
While keloid scars cannot always be entirely prevented, there are steps you can take to reduce the risk. If you are prone to keloids, avoid unnecessary piercings, tattoos, or elective surgeries. For necessary procedures, speak to a dermatologist about preventive measures such as silicone gel application, pressure dressings, or corticosteroid injections to minimise scarring.
Unlike normal scars that may fade over time, keloid scars tend to persist, and may even grow larger. Without treatment, they do not typically resolve on their own. However, there are various medical treatments available that can help shrink, flatten, and improve the appearance of keloid scars.
Yes, keloids have a tendency to recur, especially after surgical removal. To reduce the risk of recurrence, dermatologists often recommend combination treatments such as corticosteroid injections, laser therapy or radiation therapy after surgical excision.
Yes, keloid scars can be treated at any age, though treatment plans may vary depending on the patient’s skin type, age, and medical history. It is always best to consult a dermatologist to determine the most suitable treatment for your specific needs.
The timeframe for noticeable improvement depends on the treatment method used. Corticosteroid injections, laser therapy, and silicone sheets often require multiple sessions over weeks or months. Results from surgical removal or radiation therapy may become apparent sooner but require careful monitoring to prevent recurrence.

Growths on the skin or just beneath the skin can be caused by a variety of conditions, most types of bumps on the skin are caused by benign or harmless growths. Despite this, they can still cause discomfort and pain from friction, clothing, or getting caught in jewellery.
Among the common types of lumps and bumps found on the skin include:
Although most causes of lumps and bumps on the skin are benign, it is important to know when it may be indicative of a skin cancer lesion, or a lymphoma. Warning signs to look out for include:
Any concerning symptoms should prompt you to visit a healthcare provider. Early detection and treatment of cancer can be life-saving.
Some growths on the skin may resemble one another, and may even look similar to other more serious skin lesions. Hence, it is crucial that you visit a dermatologist for a proper diagnosis and avoid performing any at-home removals. Typically, your dermatologist will perform the following tests to diagnose your condition:
Most of the lumps and bumps on the skin are likely to be benign, and may not require removal or treatment if they are not painful or bothersome. You may want to remove the growths for certain reasons, including for aesthetic purposes. Depending on the type of growth, your dermatologist may use the following procedures for removal or treatment:
Ultimately, your dermatologist will decide which treatment method is the most suitable for your condition. It is important to consult with your doctor and convey your concerns and preference as well.
Skin lumps and bumps may be a cause of discomfort and can negatively impact your self-esteem. Fortunately, removal and treatment of the lesions are widely accessible. However, it is important to perform a proper check and diagnosis before undergoing any removal procedures. Certain benign growths may become cancerous and spread if the wrong treatment is performed.
If you have any doubts or concerns regarding skin lumps and bumps, or if you would like to schedule a consultation session with our dermatologists, reach out to us to book an appointment now.
Can skin growths and lesions go away over time?
These skin lesions are not likely to go away on their own and some growths may slowly grow larger. If you are not particularly bothered by it, they may be left alone. However, it is still recommended to get your lesions checked by a dermatologist to ensure that they are not harmful or malignant.
Can I remove the lumps or bumps on my own?
It is not recommended to perform removals on your own. Common risks and complications of at-home removals include infections, scarring, incomplete removal, and recurrence of the growth.
When should I see a dermatologist?
Ideally, you should visit the dermatologist any time you have any concerns of lumpy growth on or under the skin. Furthermore, if the lesion starts to become bothersome or painful, you should visit a dermatologist to discuss treatment options.
it is best to get it checked if you experience the following:
How long does it take to recover from a removal procedure?
Recovery from a removal procedure varies according to the procedure performed, as well as the size of the lump or bump removed. Minimally invasive procedures may take less time to recover fully (2 to 4 weeks), while more invasive procedures such as surgical excision for large growths may take up to 8 weeks to fully recover.
Is a skin growth removal procedure covered by MediSave or insurance?
MediSave can be used to cover expenses for skin growth removal procedures. However, it highly depends on the procedure being performed. In most cases, MediSave can be used to cover medically necessary procedures, such as for growths that are causing serious discomfort/disabling you from performing daily activities, or at risk of malignant transformation.
Typically, removal for aesthetic reasons may not be covered, as they may not be considered medically necessary. Our clinic staff is equipped to provide financial guidance, helping you understand what treatments are claimable and what falls under out-of-pocket expenses.

Moles, sometimes coined “beauty marks”, are little spots on the skin that can either add charm or raise concern. Most adults have up to 40 moles on their body, and these growths are typically harmless and can be left alone.
However, in some cases, some moles can signal changes in our skin that shouldn’t be ignored. Whether you have always had them, or a new one appears, understanding moles and what they could potentially mean for your skin health is important.
Moles, or nevi (singular: nevus), are small, dark brown spots on the skin composed of melanocytes, or pigment-forming cells [1]. Moles can be present at birth or form throughout your life. Typically, moles form in parts of the body exposed to the sun.
The exact causes of moles are not clearly understood. However, certain features in people indicate their likelihood of developing moles, these include [2]:
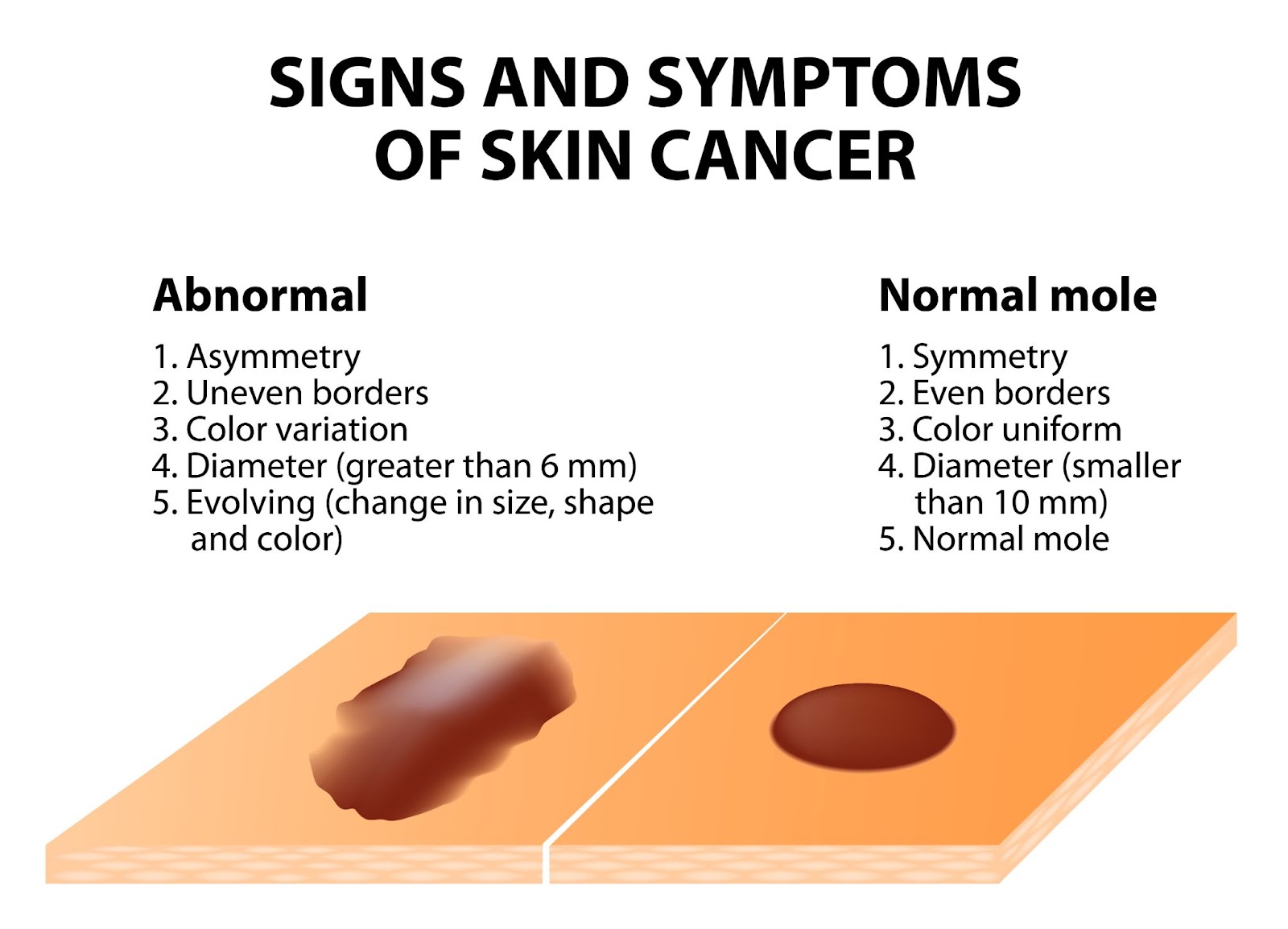
Most moles on our skin are harmless and can be left alone. However, moles can signify skin cancer. If you have a mole that you suspect is abnormal, a common guide to follow is the ABCDE guideline:
If you have moles with these characteristics, or notice these changes on a mole over a short period of time, it is highly recommended to get a dermatologist to assess the mole. Several helpful tips to take pictures and document changes of the mole include:
In addition to the features described in the ABCDE guideline, moles at risk of malignancy, or which are malignant may show the following characteristics:
In any case of doubt, it is always encouraged to visit a dermatologist for a thorough examination. Early detection of cancerous lesions allows treatment to be given early, preventing the spread of cancer cells. Once cancer has spread, it is more difficult to treat and manage, hence why early treatment can be life-saving.
Although moles are typically harmless and do not always need treatment or removal, many people opt to get them removed for the following reasons:
Typically, your dermatologist can recommend you to get a mole removed after assessment and diagnosis of the mole. A mole removal procedure can be done by the following treatments:
Before undergoing a mole removal procedure, it is important to get a proper assessment by a qualified dermatologist. Certain methods of removal, such as lasers, electrocautery, and cryotherapy, do not provide tissue samples for a biopsy. If your dermatologist suspects a mole for potential malignancy, they may recommend surgical excision, which can be followed by tissue biopsy for a proper diagnosis. Some removal methods are also at risk of mole recurrence, hence it is important to consult your dermatologist before undergoing any mole removal procedures.
After your removal procedure, your dermatologist will give you detailed instructions on how to care for the surgical wound. They may also ask you to come back for a follow-up visit to monitor your skin’s healing process, as well as to discuss biopsy results on the removed tissue if necessary.
Moles are common skin growths, are typically harmless, and do not necessarily require removal. However, there are cases where prompt assessment and removal are paramount in preventing skin cancer.
Regardless of the reason, it is always recommended to visit a dermatologist for a proper mole removal, as this limits the risk of infection, scarring, and mole recurrence. More importantly, if you experience a suspicious mole, book a consultation with us for a detailed assessment and personalised treatment plan.
Can I remove moles on my own?
Can I just have my mole removed at the spa by my therapist?
It is recommended to have your mole removed at a dermatologist’s office as it is medically supervised to ensure safe removal with sterile and precise techniques. More importantly, your mole can be properly assessed on whether it is benign or potentially cancerous — preventing risk of complications or missing a very serious condition.
When should I visit a doctor for mole removal?
Moles do not always need removal if they do not bother you, aesthetically or physically. However, if you notice abnormal changes of your mole, such as change in colour, size, and shape, or if it starts to itch, burn or feel painful, you should visit a dermatologist to get it assessed and diagnosed.
How can I prevent moles?
Some moles may not be preventable, especially if you are genetically predisposed to them. However, certain lifestyle habits can reduce mole formation, and also reduce the risk of melanoma development from moles:
Do moles get bigger with age?
Why do moles suddenly appear?
The exact reason why moles appear are not entirely understood, most moles appear in childhood or adolescence, some moles can also appear later in life which may be due to exposure to the sun. Some have also argued that hormonal changes, such as during pregnancy, causes new moles to appear. However, scientists have not found a clear relationship between pregnancy and new mole development.
How to stop moles from growing?
Benign moles are not likely to grow, and even if they did it will be very gradual over a period of several years, hence if you notice a mole growing rapidly over a short period of time, you should visit a dermatologist as it may be a sign of skin cancer. You can prevent the development of new moles by protecting your skin with sunscreen or protective clothing, as well as limiting your time outdoors.
During pregnancy, the body undergoes significant hormonal, vascular, and metabolic changes, many of which affect the skin. While some pregnancy-related skin changes gradually fade, others persist or even worsen after childbirth.
We understand that new mothers often experience a range of postpartum skin concerns, including melasma (dark patches on the face), acne, stretch marks, and increased skin sensitivity. Many also notice postpartum hair loss (telogen effluvium), which typically peaks between 3 to 6 months after giving birth, or weakened nails that become brittle or prone to splitting. Understandably, these changes can feel overwhelming, especially when combined with the physical and emotional adjustments of early motherhood.
Thankfully, many of these conditions are treatable with the right approach.

The postpartum period brings significant hormonal fluctuations that can affect the skin in multiple ways. Here are some of the common skin conditions that affect new mothers post-pregnancy:

Although many postnatal issues resolve naturally, some symptoms we experience could be telling of an underlying condition. Some signs and symptoms to look out for include:

Being a new mother in itself is a new challenge, and having to deal with the hormonal and physiological changes that come with it can be daunting. A postnatal dermatologist can provide insight on these changes, as well as medical-grade, breastfeeding-safe treatments.
Understandably, every new mother’s skin responds differently after childbirth. To provide the most personalised care, we utilise comprehensive diagnostic methods to assess postpartum skin, hair, and nail concerns accurately.
The type of treatment recommended by your dermatologist varies, depending on the type of skin concern you experience and the root cause of the issue. Some of these treatments include:
Melasma can take months to fade naturally, and in some cases, pigmentation lingers without intervention. Our treatments focus on reducing excess melanin production while protecting the skin from further darkening.
Fluctuating hormone levels, sleep deprivation, and stress can trigger postnatal acne. Treating acne postpartum requires gentle yet effective solutions that avoid harsh ingredients unsafe for breastfeeding mothers.
Stretch marks form when the skin stretches rapidly, causing collagen and elastin fibres to break. While they naturally fade over time, targeted treatments can improve texture, boost collagen production, and reduce their visibility.
Hair shedding after childbirth is common and usually self-resolving. However, for those experiencing prolonged or severe hair loss, we offer treatments to support regrowth and strengthen hair follicles.
Many women develop increased skin sensitivity, irritation, or dryness after childbirth. Maintaining a healthy skin barrier is crucial for postnatal skincare.
Post-pregnancy patients need specialised obstetric dermatological care. At Livingstone Dermatology, we understand that new mothers experience skin concerns differently, require breastfeeding-safe treatments, and have limited time for complex routines. Our dermatologist provides customised treatment plans that fit into your postnatal lifestyle, helping you feel confident in your skin once again.
If you are experiencing persistent skin, hair, or nail concerns after childbirth, schedule a consultation with us today for a detailed skin analysis and personalised postnatal treatment plan.
It’s important to review your skincare products postpartum, as certain ingredients like retinoids and high-dose salicylic acid are not recommended during breastfeeding. Opt for products with gentle, hydrating ingredients, and consult a dermatologist to ensure they’re safe for both you and your baby.
While genetics play a significant role in the development of stretch marks, maintaining skin hydration can help. Regularly applying moisturisers rich in hyaluronic acid or natural oils may improve skin elasticity. However, no topical treatment can guarantee prevention.
Yes, treatments like topical azelaic acid and vitamin C are considered safe during breastfeeding and can help lighten melasma. It’s crucial to use broad-spectrum sunscreen daily to prevent further pigmentation. Always consult a dermatologist before starting any new treatment.
Postpartum hair shedding is common and usually peaks around four months after delivery. Most women see their hair return to its normal fullness by their child’s first birthday. If hair loss continues beyond this or is causing concern, consult a dermatologist.
Postpartum skin conditions in mothers, such as eczema or melasma, do not directly affect the baby. However, if you have a contagious skin condition, it’s important to take precautions to prevent transmission. Always consult a healthcare provider for guidance.
Hormonal changes after childbirth can lead to dry skin. To manage this, use a gentle, hydrating cleanser and apply a moisturiser containing emollients, occlusives, and humectants to help maintain skin hydration. Additionally, ensure you’re drinking plenty of water, especially if you’re breastfeeding.
Yes, postpartum hormonal fluctuations can make your skin more sensitive than usual. You might react to products or environmental factors that previously didn’t affect you. Opt for fragrance-free, hypoallergenic skincare products and consult a dermatologist if sensitivities persist.
Yes, non-invasive treatments like some types of laser therapies and microneedling can help improve skin elasticity and reduce the appearance of stretch marks. Consult a dermatologist to determine the best course of action based on your specific needs.

Psoriasis is a chronic skin condition that affects millions of people worldwide, including many in Singapore. While not as widely discussed as eczema, psoriasis is a common dermatological concern, with estimates suggesting that it affects around 1% of the population.
Psoriasis can develop at any age, but it typically first appears between the ages of 15 and 35. Though psoriasis is not contagious, it can significantly impact one’s quality of life, both physically, and emotionally.
Psoriasis is an autoimmune condition where the immune system mistakenly attacks healthy skin cells, triggering rapid cell turnover. This results in the buildup of dry, scaly plaques that cause redness, itching, and discomfort. The severity of psoriasis varies, with some individuals experiencing only minor irritation, while others face widespread flare-ups that affect their quality of life. In fact, the condition tends to follow a cycle, with periods of flare-ups followed by remissions.
There are several types of psoriasis, including:
Some of the common areas, where psoriasis often develop, include:

Psoriasis is usually a combination of genetics and triggers. It is caused by an overactive immune system that mistakenly accelerates skin cell production. Normally, skin cells take about a month to renew, but in psoriasis, this process happens within days. The excess cells pile up, forming the characteristic plaques and scales.
The exact triggers vary from person to person but can include:
One of the most recognisable signs is the formation of plaques, which appear raised, thickened patches of skin covered with silvery-white scales. Additionally, some of the common symptoms include:
Psoriasis, and eczema are both chronic skin conditions that cause redness, inflammation, and itching. But they have distinct differences in their appearance, causes, and triggers. Understanding these differences can help in identifying the condition and seeking appropriate treatment.
Characteristics | Psoriasis | Eczema |
Appearance | Characterised by thick, raised plaques with well-defined borders. The affected skin often has silvery-white scales that flake off. The plaques are usually inflamed, and the skin beneath may appear shiny, and red. | Typically appears as red, inflamed or weepy patches of skin with less distinct borders. The skin may look dry, cracked, or crusted, and in some cases, it oozes clear fluid, especially during flare-ups. |
Itchiness, and Sensation | Itching can vary but is generally milder compared to eczema. Some people report a burning or stinging sensation instead. | The hallmark of eczema is intense itching, which can become unbearable, especially at night. Persistent scratching can worsen inflammation and cause the skin to thicken – a process called lichenification. |
Triggers | Triggered by an overactive immune response, leading to rapid skin cell turnover. Common triggers include infections, stress, skin injuries, and certain medications. | Often triggered by external irritants and allergens, such as soaps, detergents, pollen, dust mites or pet dander. Weather changes and emotional stress can also worsen symptoms. |
Affected Areas | Commonly appears on the scalp, elbows, knees, and lower back. It can also affect nails, causing pitting, thickening, or crumbling. | Frequently found in the creases of the elbows, and knees, as well as on the hands, neck, and face. In infants, eczema often appears on the cheeks, and scalp. |
Underlying Cause | An autoimmune condition where the immune system mistakenly speeds up skin cell production, leading to plaque buildup. | Primarily linked to a weakened skin barrier, making the skin more sensitive to allergens, and irritants. It is often associated with other allergic conditions like asthma, and hay fever. |
As with any other skin condition, psoriasis is diagnosed through a combination of several diagnostic methods, such as:

There is no permanent cure for psoriasis. However, there are a variety of treatments available to effectively manage symptoms, reduce flare-ups, and improve quality of life. The best treatment plan depends on the severity of the condition, the type of psoriasis, and individual response to therapies. At Livingstone Dermatology, treatments can include:

Psoriasis is a chronic skin condition that stems from an overactive immune system, leading to inflammation, scaling, and discomfort. While it is not contagious, it can significantly impact one’s quality of life if left unmanaged.
It goes without saying that seeking medical advice early is key to managing psoriasis effectively. A dermatologist can provide a personalised treatment plan tailored to your condition, helping to control flare-ups, and improving skin health. Schedule a consultation with us today to take the first step towards healthier, and more comfortable skin.
Currently, there is no permanent cure for psoriasis. However, various treatments can effectively manage symptoms, and reduce flare-ups. With the right approach, including medications, lifestyle adjustments, and medical therapies, many people with psoriasis can achieve long-term remission, and maintain healthy skin.
No, psoriasis is not contagious. It is an autoimmune condition, meaning it results from an overactive immune system rather than an infection. You cannot catch psoriasis from another person through physical contact, sharing personal items or exposure to skin flakes.
Yes, scratching or injuring psoriasis plaques can break the skin barrier, making it vulnerable to bacterial infections. Signs of an infection include increased redness, warmth, swelling, pus, and pain in the affected area. If you develop a fever or notice worsening symptoms, seek medical attention promptly.
Psoriasis is more than just a skin condition as it can be linked to other health concerns. Some common complications include:
While psoriasis cannot be entirely prevented, certain lifestyle habits can help reduce flare-ups, and minimise symptoms. These include:
Psoriasis can impact daily life, but with proper management, many individuals continue to live full, active, and fulfilling lives. Seeking treatment, finding emotional support, and making lifestyle adjustments can significantly improve comfort, and confidence. If psoriasis is affecting your well-being, our dermatologist can help tailor a treatment plan to suit your needs.
Yes, some people experience periods where their psoriasis symptoms disappear completely — this is known as remission. Remission can last for weeks, months or even years, depending on individual triggers, and treatment effectiveness. However, psoriasis is a chronic condition, and flare-ups may return at any time. As such, consistent management, and professional guidance are key to keeping symptoms under control.
Diet alone does not cause or cure psoriasis, but certain foods may influence inflammation levels in the body. Some individuals find that reducing processed foods, excessive sugar, and alcohol while incorporating anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids can help manage symptoms. However, dietary triggers vary from person to person, so it is best to observe how your body responds.
At Livingstone Dermatology, we understand the impact psoriasis can have on your daily life. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Rosacea is a long-term skin condition that causes persistent redness, visible blood vessels, and sometimes acne-like bumps on the face. Although it is often mistaken for common skin sensitivities or acne, rosacea is a distinct dermatological concern that requires proper management.
While the exact number of people affected in Singapore is unknown, rosacea is more prevalent among adults aged 30 to 50 years old, particularly those with fair skin. If the condition is left untreated, symptoms can worsen over time, leading to increased discomfort, and self-consciousness.

Rosacea is an inflammatory skin disorder that primarily affects the central face, including the cheeks, nose, forehead, and chin. It often begins with episodes of flushing, where the skin temporarily turns red before returning to normal.
Over time, this redness can become persistent, and small, dilated blood vessels, known as telangiectasia, may appear. Some individuals also develop bumps or pimples that resemble acne, while others experience eye irritation, known as ocular rosacea.
Although rosacea is not contagious, it can significantly impact daily life by causing discomfort, and emotional distress.
Rosacea presents in different forms, each with unique characteristics, such as:
The exact cause of rosacea is not fully understood, but it is believed to result from a combination of genetic, environmental, and immune system factors. Some of the key triggers, and risk factors include:

While symptoms vary from person to person, some of the most common signs include:
Although rosacea primarily affects the face, it can affect different parts of the face, and body, including:
Diagnosing rosacea involves a thorough assessment of your skin, symptoms, and medical history. At Livingstone Dermatology a thorough assessment of your skin condition will be made, and you may expect the following:

When it comes to the effective management of Rosacea, the treatment plan generally focuses on reducing symptoms, preventing flare-ups, and improving skin health. While there is no cure, personalised treatments at Livingstone Dermatology can help control the condition and minimise discomfort.
In conclusion, rosacea is a long-term skin condition that causes redness, visible blood vessels, and sensitivity, often triggered by environmental, and lifestyle factors. Although it is not contagious, it can worsen over time if left untreated, leading to persistent discomfort and, in some cases, complications such as thickened skin or eye irritation.
Early intervention is key to keeping rosacea under control. Our skilled, and experienced dermatologist can diagnose your specific type of rosacea, and create a personalised treatment plan to manage symptoms, and prevent flare-ups. If you are experiencing ongoing redness, sensitivity or unexplained skin changes, do not wait for them to intensify. Schedule a consultation with us today, and take the first step towards clearer, healthier skin.
Is rosacea painful?
Is rosacea an autoimmune disease?
Rosacea is not classified as an autoimmune disease, but it does involve an abnormal immune response. The condition is thought to be linked to an overactive inflammatory reaction in the skin, as well as increased sensitivity to environmental factors, and microorganisms like Demodex mites.
While the exact cause is still being researched, rosacea shares some similarities with autoimmune, and inflammatory conditions in terms of immune system involvement.
How can I differentiate a rosacea rash from a lupus rash?
Both rosacea, and lupus can cause facial redness, but there are key differences:
Can rosacea be cured permanently?
Currently, there is no permanent cure for rosacea, but the condition can be effectively managed with proper treatment, and lifestyle adjustments. Many people with rosacea see significant improvements by following a personalised treatment plan that includes topical or oral medications, laser therapy, and trigger avoidance. Early diagnosis, and treatment can help prevent symptoms from worsening over time.
Can rosacea be prevented?
Since rosacea has a genetic and environmental component, it cannot always be entirely prevented. However, flare-ups can be minimised by identifying, and avoiding triggers such as excessive sun exposure, alcohol, spicy foods, and stress. Consistently using gentle skincare products, wearing daily sun protection, and following a dermatologist-recommended treatment plan can help keep rosacea symptoms under control.
If I have rosacea, does that mean I cannot wear makeup?
You can still wear makeup if you have rosacea, but it is important to choose products that are gentle, non-comedogenic, and free from irritating ingredients such as alcohol, fragrance, and harsh preservatives.
Additionally, look for mineral-based foundations, green-tinted primers to neutralise redness, and hydrating formulas that support skin health. On top of that, always remove makeup with a gentle, non-stripping cleanser to avoid aggravating your skin.
If you are unsure of the type of makeup or skincare products you should use, our dermatologist can recommend suitable makeup, and skincare options tailored to your skin’s needs.

A skin allergy is a condition in which the immune system reacts abnormally to a substance that is typically harmless, leading to inflammation and discomfort. When an allergic reaction occurs, the skin may develop redness, swelling, itching, rashes, or even blisters.
The way a skin allergy presents depends on the type of reaction, with some conditions causing immediate flare-ups, while others develop gradually over time. Below are some of the most common types of skin allergies:
Type | Description |
Contact Dermatitis | Occurs when the skin comes into direct contact with an allergen, leading to redness, itching, and irritation. Common triggers include nickel, fragrances, cosmetics, latex, and certain plants like poison ivy. |
Atopic Dermatitis (Eczema) | A chronic condition that causes dry, itchy, and inflamed skin. While often linked to genetics and environmental factors, allergens can worsen symptoms. It is common in children but may persist into adulthood. |
Urticaria (Hives) | Characterised by raised, red, and itchy welts that appear suddenly due to an allergic reaction to foods, medications, insect stings, or environmental triggers. Hives can be acute (lasting hours or days) or chronic (lasting for weeks or longer). |
Angioedema | A deeper form of swelling that affects the skin and mucous membranes, often occurring around the eyes, lips, hands, and feet. It may accompany hives and, in severe cases, can impact breathing, which may require immediate medical attention. |

A skin allergy occurs when the immune system mistakenly identifies a harmless substance as a threat and initiates a defensive response. This process begins when the skin encounters an allergen, prompting specialised immune cells called Langerhans cells to capture and present it to T-cells in the lymph nodes. If the immune system perceives the substance as harmful, it triggers the release of inflammatory chemicals, such as histamines and cytokines. These chemicals cause blood vessels to dilate, increasing blood flow to the affected area and leading to redness, swelling, and itching.
In some cases, the reaction occurs immediately, as seen in conditions like urticaria, while in others, such as allergic contact dermatitis, it may take hours or days to develop. Over time, repeated exposure to the allergen can intensify the immune response, making future reactions more severe. This hypersensitivity mechanism is what differentiates allergic reactions from simple irritant responses, which do not involve the immune system.
The symptoms of a skin allergy vary depending on the type of reaction and the severity of the immune response. Some symptoms appear immediately after exposure to an allergen, while others develop gradually over time. Common signs of a skin allergy include:
Symptoms can range from mild discomfort to more severe cases that require immediate medical attention, especially if swelling affects breathing or spreads extensively across the body.

Certain individuals are more susceptible to developing skin allergies due to a combination of genetic, environmental, and lifestyle factors. In Singapore, where high humidity and urban pollutants are common, some risk factors can further increase the likelihood of allergic skin reactions. These include:
Recognising these risk factors can help individuals take preventive measures to reduce their chances of experiencing allergic flare-ups.
Since allergic reactions can vary widely from person to person, we use varied diagnostic methods to pinpoint the exact cause of your symptoms. Our dermatologists assess your medical history, lifestyle factors, and environmental exposures before recommending specific tests to identify potential allergens.
Common diagnostic methods include:
Our dermatologists use a combination of medical therapies, skincare recommendations, and lifestyle adjustments to help you achieve long-term relief. Treatment options may include:
If you are experiencing persistent skin irritation, unexplained rashes, or allergic flare-ups, schedule a consultation with us for a detailed diagnosis and personalised treatment solutions.
While there is no definitive cure for skin allergies, effective management is possible through identifying and avoiding triggers, using appropriate medications, and following a proper skincare routine. Many individuals experience significant relief and may have prolonged periods without symptoms.
No, skin allergies are not contagious. They result from an individual’s immune response to specific allergens and cannot be transmitted from person to person.
Stress does not directly cause skin allergies, but it can exacerbate existing conditions. Managing stress through relaxation techniques and lifestyle changes may help reduce flare-ups.
Preventing flare-ups involves identifying and avoiding known allergens, maintaining a regular skincare routine with hypoallergenic products, and protecting your skin from environmental factors like extreme temperatures and pollutants.
Over-the-counter creams, such as hydrocortisone, can provide temporary relief for mild symptoms. However, it’s essential to consult a dermatologist for persistent or severe reactions to ensure appropriate treatment.
Certain foods may trigger or worsen skin allergies in susceptible individuals. Keeping a food diary and observing any correlations between diet and skin reactions can be helpful. Consulting a healthcare professional is recommended for personalised advice.
If you experience persistent, severe, or worsening symptoms, or if over-the-counter treatments do not provide relief, it’s advisable to consult a dermatologist. Professional evaluation can help identify specific allergens and develop an effective treatment plan.
At Livingstone Dermatology, we understand the impact skin allergies can have on your daily life. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of various types of skin cancers. Our experienced dermatologist offers expert care to ensure early detection, accurate diagnosis, and effective treatment for optimal outcomes.
Basal Cell Carcinoma (BCC): This is the most common form of skin cancer, typically appearing as a pearly or waxy bump, often with visible blood vessels.
Squamous Cell Carcinoma (SCC): SCC often appears as a red, scaly patch, a raised growth with a central depression, or a wart-like growth.
Melanoma: Melanoma is a less common but more aggressive form of skin cancer, often characterized by irregularly shaped moles with uneven coloring.
Actinic Keratosis (AK): Although not cancer itself, AKs are considered precancerous and can develop into SCC if left untreated.
Merkel Cell Carcinoma: This is a rare, aggressive form of skin cancer that usually appears as a painless, firm, and fast-growing nodule.
Early detection of skin cancer is crucial for successful treatment. Our dermatologists conduct thorough examinations, often supplemented by advanced imaging or biopsy techniques, to accurately diagnose and stage skin cancers.
At Livingstone Dermatology, we prioritize your skin health and overall well-being. Our experienced dermatologist is dedicated to providing expert care for individuals with skin cancers, guiding you through the diagnosis and treatment process with compassion and expertise.
Livingstone Dermatology specializes in the diagnosis and treatment of warts and verrucas. Our experienced dermatologists offer expert care to ensure effective removal and provide guidance on preventing recurrence.
Warts: Warts are non-cancerous growths caused by the human papillomavirus (HPV). They can appear anywhere on the body, often on the hands, feet, and face. Warts are typically small, rough, and may have a cauliflower-like appearance.
Verrucas (Plantar Warts): Verrucas are a type of wart that specifically develop on the soles of the feet. They may appear flat or have a rough, bumpy surface, often surrounded by hardened skin.
Warts and verrucas are highly contagious and can be contracted through direct or indirect contact with the virus. Common sources of infection include:
Our dermatologist provides guidance on preventive measures, such as avoiding direct contact with warts, keeping feet clean and dry, and wearing protective footwear in public areas.
At Livingstone Dermatology, we understand the discomfort and frustration that warts and verrucas can cause. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of urticaria, commonly known as hives. Our experienced dermatologists offer expert care to help you identify triggers and manage symptoms effectively.
Urticaria, more commonly known as hives, is a skin condition characterized by raised, itchy welts that can appear anywhere on the body. These welts often have defined borders and can vary in size and shape. Urticaria can be acute (lasting less than six weeks) or chronic (lasting longer than six weeks).
Urticaria can be triggered by a wide range of factors, including:
Our dermatologist conducts thorough evaluations to accurately diagnose urticaria and identify potential triggers. Treatment options may include:
While urticaria can be a chronic condition, with the right treatment and lifestyle modifications, it can be effectively managed. Our experienced dermatologists will work closely with you to develop a personalized treatment plan that addresses your specific needs and lifestyle.
At Livingstone Dermatology, we understand the discomfort and frustration that urticaria can cause. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of vitiligo, a skin condition characterized by the loss of natural skin color. Our experienced dermatologists offer expert care to help you understand and manage this condition effectively.
Vitiligo is a chronic skin condition that results in the loss of pigmentation, leading to the development of white patches on the skin. It occurs when the melanocytes, the cells responsible for producing melanin (skin pigment), are destroyed or stop functioning.
While the exact cause of vitiligo is not fully understood, it is believed to be related to a combination of genetic, autoimmune, and environmental factors. Certain triggers, such as stress, trauma, or illness, may exacerbate the condition.
Our dermatologist understands the impact vitiligo can have on self-esteem and body image. We provide support and guidance on living well with vitiligo, including skincare recommendations and advice on sun protection.
At Livingstone Dermatology, we are dedicated to providing expert care for individuals with vitiligo. Our experienced dermatologist works closely with you to develop a personalized treatment plan that addresses your specific needs and concerns.
Corns and calluses are common skin conditions caused by repeated friction or pressure on specific areas of the skin. They typically form on the feet and hands as a protective response to prevent further irritation.
Corns often develop on the tops and sides of toes, or on the sole of the foot, as a result of ill-fitting shoes, abnormal gait, or deformities like hammertoe. Calluses, on the other hand, typically form on the palms, fingers, or soles of the feet due to repetitive actions or pressure.
To prevent the recurrence of corns and calluses, it’s essential to continue wearing well-fitting shoes, using orthotics if recommended, and maintaining good foot hygiene.
Livingstone Dermatology provides comprehensive care for corns and calluses. Our experienced dermatologist will assess your condition and recommend a personalized treatment plan to alleviate discomfort and help you achieve healthy, pain-free skin.
Cysts and abscesses are common skin conditions characterized by the formation of enclosed pockets of fluid, pus, or other materials within or beneath the skin. While they may appear similar, they have distinct characteristics and treatment approaches.
Cysts are closed sacs filled with fluid, semi-solid material, or air. They can develop anywhere on the body and vary in size. Cysts are typically non-cancerous and can be caused by a variety of factors, including infection, blockage of ducts, or genetic predisposition.
Abscesses, on the other hand, are localized infections that result in the accumulation of pus. They often occur in response to bacterial infections, usually as a result of a wound or hair follicle infection. Abscesses are characterized by redness, swelling, pain, and often have a visible “head” or opening.
Proper wound care, maintaining good hygiene, and seeking prompt treatment for any skin infections can help prevent the recurrence of cysts and abscesses.
Livingstone Dermatology offers specialized care for cysts and abscesses. Our experienced dermatologist will assess your condition and recommend a personalized treatment plan to promote healing and prevent future occurrences.
Eczema, also known as dermatitis, is a common skin condition characterized by red, itchy, and inflamed skin. It often appears in patches and can range from mild to severe. Livingstone Dermatology is here to provide comprehensive care and relief for individuals dealing with eczema.
Eczema is a chronic skin condition that results from a combination of genetic and environmental factors. It is characterized by inflammation of the skin’s outer layer, leading to symptoms such as redness, itching, and the development of dry, scaly patches.
While the exact cause of eczema is not fully understood, it is believed to be related to a combination of factors, including genetics, an overactive immune response, and environmental triggers like allergens or irritants.
In addition to medical treatments, adopting a consistent skincare routine and avoiding known triggers can significantly improve the management of eczema.
At Livingstone Dermatology, our experienced dermatologist is dedicated to providing personalized care for individuals with eczema. We work closely with each patient to develop a customized treatment plan aimed at providing relief and improving the overall health of the skin.

Sweating is a normal bodily function that helps regulate temperature. However, for some individuals, excessive sweating occurs regardless of temperature or physical activity. This condition, known as hyperhidrosis, affects daily life, causing discomfort, and social anxiety. Fortunately, various treatments are available to help manage excessive sweating effectively.
Hyperhidrosis is a medical condition characterised by excessive sweating that goes beyond what is necessary for temperature regulation. It can affect different parts of the body, including the palms, soles, underarms, and face. This condition is typically caused by overactive sweat glands, leading to persistent sweating – even when at rest.
Hyperhidrosis is categorised into two main types, which are:
The overstimulation of the sweat glands, due to the influence of the nervous system, is typically the cause of hyperhidrosis. Be that as it may, the causes can be divided into two categories:

Some of the common symptoms of hyperhidrosis are:
Beyond physical discomfort, hyperhidrosis can significantly impact daily life, and mental well-being:
The eccrine glands are responsible for producing sweat. As it exists in the skin throughout the body, symptoms of hyperhidrosis can occur anywhere, with the following areas being the primary areas:
When it comes to hyperhidrosis, it is important to manage the triggers. There are certain factors that can worsen hyperhidrosis episodes, including:

Diagnosing hyperhidrosis involves a thorough evaluation to determine the type, severity, and potential underlying causes of excessive sweating. At Livingstone Dermatology, our dermatologists begin with a detailed consultation, and physical examination.
During the initial consultation, our dermatologists will assess your symptoms through:
In addition to a physical examination, our dermatologists may recommend specific tests to confirm the diagnosis, and assess the severity of the condition:
Treatment for hyperhidrosis is primarily focused on managing the condition, and preventing it from exacerbating. As such, it includes a variety of treatment options, ranging from conservative measures to more invasive forms of medical intervention – all of which are tailored specifically to each patient.
For mild to moderate hyperhidrosis, conservative methods can help manage excessive sweating:

For moderate to severe hyperhidrosis, medical treatments offer longer-lasting relief:
For severe hyperhidrosis that does not respond to other treatments, surgical interventions may be considered:
Excessive sweating can be disruptive, and challenging to manage on your own. Thankfully, there are several medical-grade treatments that can help you manage hyperhidrosis symptoms effectively.
Schedule a consultation today for a detailed diagnosis and personalised treatment plan.
Normal sweating occurs as a natural response to heat, physical activity or emotional stress, helping to regulate body temperature. It usually stops once the triggering factor subsides.
Excessive sweating, on the other hand, happens regardless of external conditions, and can interfere with daily activities. The key differences include:
Hyperhidrosis affects approximately 2 – 3% of the global population, with many cases remaining undiagnosed or untreated. This is largely due to a lack of awareness, and education related to the condition.
Most people with hyperhidrosis do not experience body odour. However, to prevent body odour (bromhidrosis), you can:
There is no conclusive evidence linking regular use of these products to breast cancer. Many formulations, including natural and clinical-strength options, are available, allowing individuals to choose what suits them best.
It is important to seek medical attention for hyperhidrosis to prevent the following potential complications:
Although treatment-related side effects are uncommon, it is important to be aware of the potential side effects. These side effects depend on the treatment method, but may include:
It is important to understand that most treatments provide temporary relief. As such, it requires repeated sessions or long-term management. However, surgical options may offer a permanent solution, but they do come with their own set of risks.
While hyperhidrosis itself may not be preventable, triggers can be managed through lifestyle adjustments, appropriate treatments.
Yes, some lifestyle adjustments can help. This includes:
Living with hyperhidrosis can be challenging, but effective treatment options are available. Our experienced dermatologist will work with you to develop a personalized treatment plan that addresses your specific concerns and provides lasting relief.

Scars are our body’s way of protecting us after the skin is injured. When the dermis is damaged, our body produces collagen fibres to repair the wound. This is laid down rapidly and densely, creating a scar.
However, when excess collagen is produced during the healing process, keloid scars can form. These are raised scars that form beyond the original wound — thick, raised, and sometimes, darker than the surrounding skin. While they do not pose serious health risks, their appearance, and potential discomfort can be distressing. Fortunately, various treatments are available to help reduce, and manage keloid scars, restoring both skin appearance and self-assurance.
Keloid scars are an overgrowth of scar tissue that forms at the site of a skin injury. Unlike regular scars, keloids extend beyond the original wound, and may continue to grow over time. This occurs due to excessive collagen production during the healing process. Instead of gradually fading, keloid scars become thick, raised, and sometimes itchy or uncomfortable. They can develop after minor skin injuries such as cuts, burns, acne or even piercings. Although harmless, their noticeable appearance can be a cosmetic concern for many individuals.
Identifying, and differentiating keloid scars is essential for seeking the right treatment. In fact, understanding their unique characteristics can help individuals determine the most ideal course of action.
Keloids can appear anywhere on the body but are more common in areas with high skin tension, and movement, including:
Keloid scars have distinct visual, and physical characteristics, such as:
Keloids form when the body produces excessive collagen while healing an injury. Collagen is a structural protein that helps repair, and strengthen the skin. However, in some individuals, an overproduction of collagen leads to the formation of keloid scars. Unfortunately, the exact reason behind this excessive collagen production remains unclear.
Keloids may develop after various skin injuries or conditions, including:

In addition to medical treatments, adopting a consistent skincare routine and avoiding known triggers can significantly improve the management of eczema.
The symptoms of keloid scars can vary but often include:
Although anyone can have keloid scars, there are certain individuals that are more prone to developing keloid scars due to genetic, and environmental factors. The risk factors include:
Several methods for assessing keloid scars include:

Treatment for keloid scars is tailored based on the severity, size, and location of the scar. At Livingstone Dermatology, our dermatologists may recommend one or a combination of the following treatment options:
While keloid scars can be persistent, and impact self-confidence, they are manageable with the right treatment approach. It is important to remember that early intervention is key to preventing excessive scar growth. At Livingstone Dermatology, we offer comprehensive keloid scar assessments, and medical-grade treatment options to help you achieve smoother, healthier skin. Contact us today for a personalised treatment plan.
Keloids are often mistaken for hypertrophic scars, a more common type of scarring. Hypertrophic scars are typically flat and vary in colour from pink to brown. They are smaller than keloids and, unlike keloids, may gradually fade over time.
Both men and women experience hypertrophic scars at similar rates, and they can affect individuals of all skin tones. These scars often result from physical or chemical injuries, such as piercings or exposure to harsh substances. Initially, hypertrophic scars may be itchy or painful, but these symptoms generally lessen as the skin heals.
Keloid scars are not always painful, but some people may experience discomfort, tenderness or itching in the affected area. The severity of symptoms varies from person to person, and larger keloids may cause more noticeable discomfort.
If pain or irritation is affecting your daily life, treatment options are available to help relieve symptoms and improve the appearance of the scar.
While keloid scars are not harmful to your overall health, they can sometimes lead to discomfort, restricted movement (if they develop over joints) or emotional distress due to their appearance. Additionally, keloids can sometimes continue to grow over time.
Most keloid treatments involve minimal downtime. Procedures like corticosteroid injections, laser therapy, and cryotherapy allow patients to resume normal activities almost immediately. However, surgical removal or radiation therapy may require a brief recovery period.
While keloid scars cannot always be entirely prevented, there are steps you can take to reduce the risk. If you are prone to keloids, avoid unnecessary piercings, tattoos, or elective surgeries. For necessary procedures, speak to a dermatologist about preventive measures such as silicone gel application, pressure dressings, or corticosteroid injections to minimise scarring.
Unlike normal scars that may fade over time, keloid scars tend to persist, and may even grow larger. Without treatment, they do not typically resolve on their own. However, there are various medical treatments available that can help shrink, flatten, and improve the appearance of keloid scars.
Yes, keloids have a tendency to recur, especially after surgical removal. To reduce the risk of recurrence, dermatologists often recommend combination treatments such as corticosteroid injections, laser therapy or radiation therapy after surgical excision.
Yes, keloid scars can be treated at any age, though treatment plans may vary depending on the patient’s skin type, age, and medical history. It is always best to consult a dermatologist to determine the most suitable treatment for your specific needs.
The timeframe for noticeable improvement depends on the treatment method used. Corticosteroid injections, laser therapy, and silicone sheets often require multiple sessions over weeks or months. Results from surgical removal or radiation therapy may become apparent sooner but require careful monitoring to prevent recurrence.

Growths on the skin or just beneath the skin can be caused by a variety of conditions, most types of bumps on the skin are caused by benign or harmless growths. Despite this, they can still cause discomfort and pain from friction, clothing, or getting caught in jewellery.
Among the common types of lumps and bumps found on the skin include:
Although most causes of lumps and bumps on the skin are benign, it is important to know when it may be indicative of a skin cancer lesion, or a lymphoma. Warning signs to look out for include:
Any concerning symptoms should prompt you to visit a healthcare provider. Early detection and treatment of cancer can be life-saving.
Some growths on the skin may resemble one another, and may even look similar to other more serious skin lesions. Hence, it is crucial that you visit a dermatologist for a proper diagnosis and avoid performing any at-home removals. Typically, your dermatologist will perform the following tests to diagnose your condition:
Most of the lumps and bumps on the skin are likely to be benign, and may not require removal or treatment if they are not painful or bothersome. You may want to remove the growths for certain reasons, including for aesthetic purposes. Depending on the type of growth, your dermatologist may use the following procedures for removal or treatment:
Ultimately, your dermatologist will decide which treatment method is the most suitable for your condition. It is important to consult with your doctor and convey your concerns and preference as well.
Skin lumps and bumps may be a cause of discomfort and can negatively impact your self-esteem. Fortunately, removal and treatment of the lesions are widely accessible. However, it is important to perform a proper check and diagnosis before undergoing any removal procedures. Certain benign growths may become cancerous and spread if the wrong treatment is performed.
If you have any doubts or concerns regarding skin lumps and bumps, or if you would like to schedule a consultation session with our dermatologists, reach out to us to book an appointment now.
Can skin growths and lesions go away over time?
These skin lesions are not likely to go away on their own and some growths may slowly grow larger. If you are not particularly bothered by it, they may be left alone. However, it is still recommended to get your lesions checked by a dermatologist to ensure that they are not harmful or malignant.
Can I remove the lumps or bumps on my own?
It is not recommended to perform removals on your own. Common risks and complications of at-home removals include infections, scarring, incomplete removal, and recurrence of the growth.
When should I see a dermatologist?
Ideally, you should visit the dermatologist any time you have any concerns of lumpy growth on or under the skin. Furthermore, if the lesion starts to become bothersome or painful, you should visit a dermatologist to discuss treatment options.
it is best to get it checked if you experience the following:
How long does it take to recover from a removal procedure?
Recovery from a removal procedure varies according to the procedure performed, as well as the size of the lump or bump removed. Minimally invasive procedures may take less time to recover fully (2 to 4 weeks), while more invasive procedures such as surgical excision for large growths may take up to 8 weeks to fully recover.
Is a skin growth removal procedure covered by MediSave or insurance?
MediSave can be used to cover expenses for skin growth removal procedures. However, it highly depends on the procedure being performed. In most cases, MediSave can be used to cover medically necessary procedures, such as for growths that are causing serious discomfort/disabling you from performing daily activities, or at risk of malignant transformation.
Typically, removal for aesthetic reasons may not be covered, as they may not be considered medically necessary. Our clinic staff is equipped to provide financial guidance, helping you understand what treatments are claimable and what falls under out-of-pocket expenses.

Moles, sometimes coined “beauty marks”, are little spots on the skin that can either add charm or raise concern. Most adults have up to 40 moles on their body, and these growths are typically harmless and can be left alone.
However, in some cases, some moles can signal changes in our skin that shouldn’t be ignored. Whether you have always had them, or a new one appears, understanding moles and what they could potentially mean for your skin health is important.
Moles, or nevi (singular: nevus), are small, dark brown spots on the skin composed of melanocytes, or pigment-forming cells [1]. Moles can be present at birth or form throughout your life. Typically, moles form in parts of the body exposed to the sun.
The exact causes of moles are not clearly understood. However, certain features in people indicate their likelihood of developing moles, these include [2]:
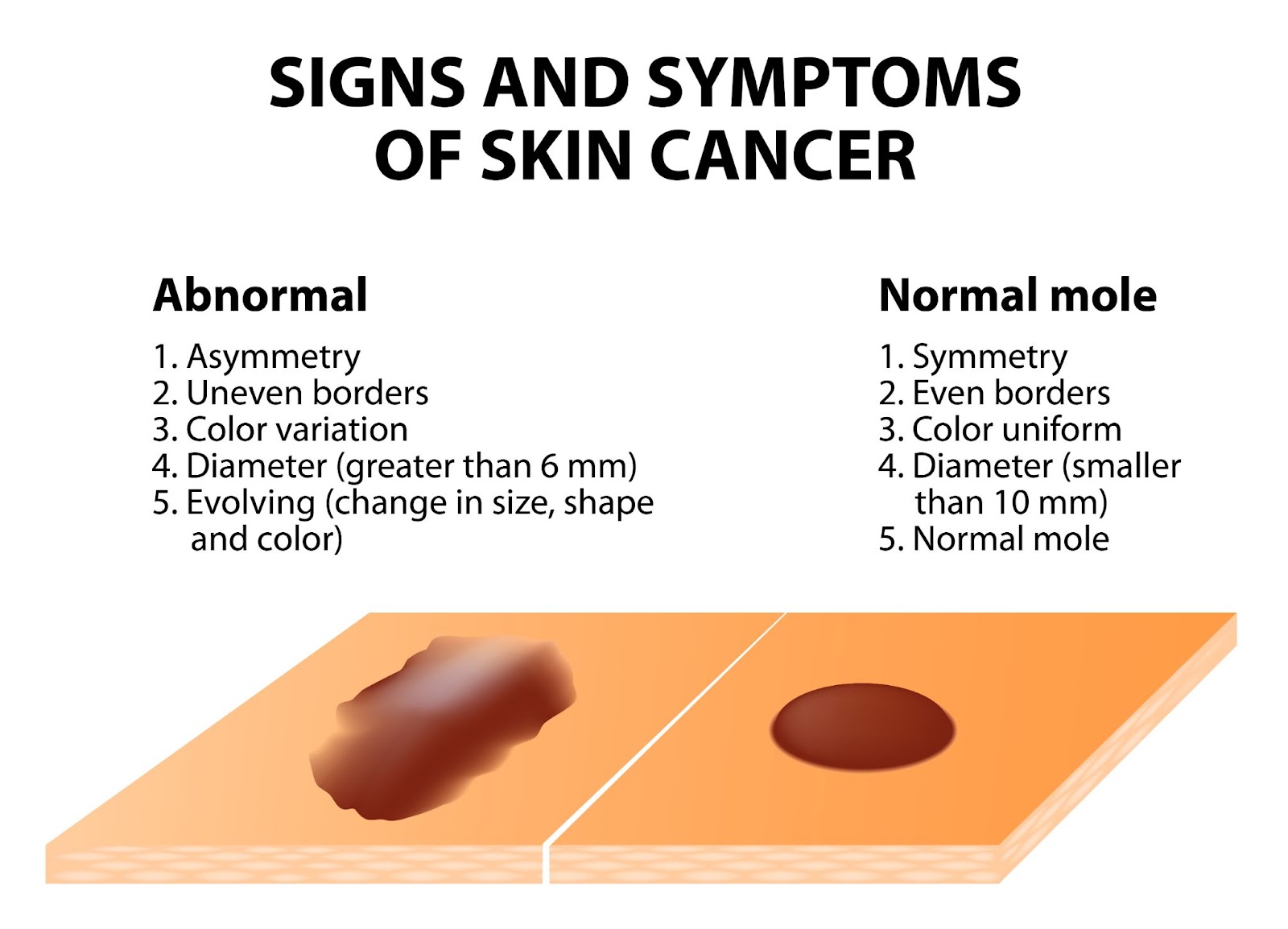
Most moles on our skin are harmless and can be left alone. However, moles can signify skin cancer. If you have a mole that you suspect is abnormal, a common guide to follow is the ABCDE guideline:
If you have moles with these characteristics, or notice these changes on a mole over a short period of time, it is highly recommended to get a dermatologist to assess the mole. Several helpful tips to take pictures and document changes of the mole include:
In addition to the features described in the ABCDE guideline, moles at risk of malignancy, or which are malignant may show the following characteristics:
In any case of doubt, it is always encouraged to visit a dermatologist for a thorough examination. Early detection of cancerous lesions allows treatment to be given early, preventing the spread of cancer cells. Once cancer has spread, it is more difficult to treat and manage, hence why early treatment can be life-saving.
Although moles are typically harmless and do not always need treatment or removal, many people opt to get them removed for the following reasons:
Typically, your dermatologist can recommend you to get a mole removed after assessment and diagnosis of the mole. A mole removal procedure can be done by the following treatments:
Before undergoing a mole removal procedure, it is important to get a proper assessment by a qualified dermatologist. Certain methods of removal, such as lasers, electrocautery, and cryotherapy, do not provide tissue samples for a biopsy. If your dermatologist suspects a mole for potential malignancy, they may recommend surgical excision, which can be followed by tissue biopsy for a proper diagnosis. Some removal methods are also at risk of mole recurrence, hence it is important to consult your dermatologist before undergoing any mole removal procedures.
After your removal procedure, your dermatologist will give you detailed instructions on how to care for the surgical wound. They may also ask you to come back for a follow-up visit to monitor your skin’s healing process, as well as to discuss biopsy results on the removed tissue if necessary.
Moles are common skin growths, are typically harmless, and do not necessarily require removal. However, there are cases where prompt assessment and removal are paramount in preventing skin cancer.
Regardless of the reason, it is always recommended to visit a dermatologist for a proper mole removal, as this limits the risk of infection, scarring, and mole recurrence. More importantly, if you experience a suspicious mole, book a consultation with us for a detailed assessment and personalised treatment plan.
Can I remove moles on my own?
Can I just have my mole removed at the spa by my therapist?
It is recommended to have your mole removed at a dermatologist’s office as it is medically supervised to ensure safe removal with sterile and precise techniques. More importantly, your mole can be properly assessed on whether it is benign or potentially cancerous — preventing risk of complications or missing a very serious condition.
When should I visit a doctor for mole removal?
Moles do not always need removal if they do not bother you, aesthetically or physically. However, if you notice abnormal changes of your mole, such as change in colour, size, and shape, or if it starts to itch, burn or feel painful, you should visit a dermatologist to get it assessed and diagnosed.
How can I prevent moles?
Some moles may not be preventable, especially if you are genetically predisposed to them. However, certain lifestyle habits can reduce mole formation, and also reduce the risk of melanoma development from moles:
Do moles get bigger with age?
Why do moles suddenly appear?
The exact reason why moles appear are not entirely understood, most moles appear in childhood or adolescence, some moles can also appear later in life which may be due to exposure to the sun. Some have also argued that hormonal changes, such as during pregnancy, causes new moles to appear. However, scientists have not found a clear relationship between pregnancy and new mole development.
How to stop moles from growing?
Benign moles are not likely to grow, and even if they did it will be very gradual over a period of several years, hence if you notice a mole growing rapidly over a short period of time, you should visit a dermatologist as it may be a sign of skin cancer. You can prevent the development of new moles by protecting your skin with sunscreen or protective clothing, as well as limiting your time outdoors.
During pregnancy, the body undergoes significant hormonal, vascular, and metabolic changes, many of which affect the skin. While some pregnancy-related skin changes gradually fade, others persist or even worsen after childbirth.
We understand that new mothers often experience a range of postpartum skin concerns, including melasma (dark patches on the face), acne, stretch marks, and increased skin sensitivity. Many also notice postpartum hair loss (telogen effluvium), which typically peaks between 3 to 6 months after giving birth, or weakened nails that become brittle or prone to splitting. Understandably, these changes can feel overwhelming, especially when combined with the physical and emotional adjustments of early motherhood.
Thankfully, many of these conditions are treatable with the right approach.

The postpartum period brings significant hormonal fluctuations that can affect the skin in multiple ways. Here are some of the common skin conditions that affect new mothers post-pregnancy:

Although many postnatal issues resolve naturally, some symptoms we experience could be telling of an underlying condition. Some signs and symptoms to look out for include:

Being a new mother in itself is a new challenge, and having to deal with the hormonal and physiological changes that come with it can be daunting. A postnatal dermatologist can provide insight on these changes, as well as medical-grade, breastfeeding-safe treatments.
Understandably, every new mother’s skin responds differently after childbirth. To provide the most personalised care, we utilise comprehensive diagnostic methods to assess postpartum skin, hair, and nail concerns accurately.
The type of treatment recommended by your dermatologist varies, depending on the type of skin concern you experience and the root cause of the issue. Some of these treatments include:
Melasma can take months to fade naturally, and in some cases, pigmentation lingers without intervention. Our treatments focus on reducing excess melanin production while protecting the skin from further darkening.
Fluctuating hormone levels, sleep deprivation, and stress can trigger postnatal acne. Treating acne postpartum requires gentle yet effective solutions that avoid harsh ingredients unsafe for breastfeeding mothers.
Stretch marks form when the skin stretches rapidly, causing collagen and elastin fibres to break. While they naturally fade over time, targeted treatments can improve texture, boost collagen production, and reduce their visibility.
Hair shedding after childbirth is common and usually self-resolving. However, for those experiencing prolonged or severe hair loss, we offer treatments to support regrowth and strengthen hair follicles.
Many women develop increased skin sensitivity, irritation, or dryness after childbirth. Maintaining a healthy skin barrier is crucial for postnatal skincare.
Post-pregnancy patients need specialised obstetric dermatological care. At Livingstone Dermatology, we understand that new mothers experience skin concerns differently, require breastfeeding-safe treatments, and have limited time for complex routines. Our dermatologist provides customised treatment plans that fit into your postnatal lifestyle, helping you feel confident in your skin once again.
If you are experiencing persistent skin, hair, or nail concerns after childbirth, schedule a consultation with us today for a detailed skin analysis and personalised postnatal treatment plan.
It’s important to review your skincare products postpartum, as certain ingredients like retinoids and high-dose salicylic acid are not recommended during breastfeeding. Opt for products with gentle, hydrating ingredients, and consult a dermatologist to ensure they’re safe for both you and your baby.
While genetics play a significant role in the development of stretch marks, maintaining skin hydration can help. Regularly applying moisturisers rich in hyaluronic acid or natural oils may improve skin elasticity. However, no topical treatment can guarantee prevention.
Yes, treatments like topical azelaic acid and vitamin C are considered safe during breastfeeding and can help lighten melasma. It’s crucial to use broad-spectrum sunscreen daily to prevent further pigmentation. Always consult a dermatologist before starting any new treatment.
Postpartum hair shedding is common and usually peaks around four months after delivery. Most women see their hair return to its normal fullness by their child’s first birthday. If hair loss continues beyond this or is causing concern, consult a dermatologist.
Postpartum skin conditions in mothers, such as eczema or melasma, do not directly affect the baby. However, if you have a contagious skin condition, it’s important to take precautions to prevent transmission. Always consult a healthcare provider for guidance.
Hormonal changes after childbirth can lead to dry skin. To manage this, use a gentle, hydrating cleanser and apply a moisturiser containing emollients, occlusives, and humectants to help maintain skin hydration. Additionally, ensure you’re drinking plenty of water, especially if you’re breastfeeding.
Yes, postpartum hormonal fluctuations can make your skin more sensitive than usual. You might react to products or environmental factors that previously didn’t affect you. Opt for fragrance-free, hypoallergenic skincare products and consult a dermatologist if sensitivities persist.
Yes, non-invasive treatments like some types of laser therapies and microneedling can help improve skin elasticity and reduce the appearance of stretch marks. Consult a dermatologist to determine the best course of action based on your specific needs.

Psoriasis is a chronic skin condition that affects millions of people worldwide, including many in Singapore. While not as widely discussed as eczema, psoriasis is a common dermatological concern, with estimates suggesting that it affects around 1% of the population.
Psoriasis can develop at any age, but it typically first appears between the ages of 15 and 35. Though psoriasis is not contagious, it can significantly impact one’s quality of life, both physically, and emotionally.
Psoriasis is an autoimmune condition where the immune system mistakenly attacks healthy skin cells, triggering rapid cell turnover. This results in the buildup of dry, scaly plaques that cause redness, itching, and discomfort. The severity of psoriasis varies, with some individuals experiencing only minor irritation, while others face widespread flare-ups that affect their quality of life. In fact, the condition tends to follow a cycle, with periods of flare-ups followed by remissions.
There are several types of psoriasis, including:
Some of the common areas, where psoriasis often develop, include:

Psoriasis is usually a combination of genetics and triggers. It is caused by an overactive immune system that mistakenly accelerates skin cell production. Normally, skin cells take about a month to renew, but in psoriasis, this process happens within days. The excess cells pile up, forming the characteristic plaques and scales.
The exact triggers vary from person to person but can include:
One of the most recognisable signs is the formation of plaques, which appear raised, thickened patches of skin covered with silvery-white scales. Additionally, some of the common symptoms include:
Psoriasis, and eczema are both chronic skin conditions that cause redness, inflammation, and itching. But they have distinct differences in their appearance, causes, and triggers. Understanding these differences can help in identifying the condition and seeking appropriate treatment.
Characteristics | Psoriasis | Eczema |
Appearance | Characterised by thick, raised plaques with well-defined borders. The affected skin often has silvery-white scales that flake off. The plaques are usually inflamed, and the skin beneath may appear shiny, and red. | Typically appears as red, inflamed or weepy patches of skin with less distinct borders. The skin may look dry, cracked, or crusted, and in some cases, it oozes clear fluid, especially during flare-ups. |
Itchiness, and Sensation | Itching can vary but is generally milder compared to eczema. Some people report a burning or stinging sensation instead. | The hallmark of eczema is intense itching, which can become unbearable, especially at night. Persistent scratching can worsen inflammation and cause the skin to thicken – a process called lichenification. |
Triggers | Triggered by an overactive immune response, leading to rapid skin cell turnover. Common triggers include infections, stress, skin injuries, and certain medications. | Often triggered by external irritants and allergens, such as soaps, detergents, pollen, dust mites or pet dander. Weather changes and emotional stress can also worsen symptoms. |
Affected Areas | Commonly appears on the scalp, elbows, knees, and lower back. It can also affect nails, causing pitting, thickening, or crumbling. | Frequently found in the creases of the elbows, and knees, as well as on the hands, neck, and face. In infants, eczema often appears on the cheeks, and scalp. |
Underlying Cause | An autoimmune condition where the immune system mistakenly speeds up skin cell production, leading to plaque buildup. | Primarily linked to a weakened skin barrier, making the skin more sensitive to allergens, and irritants. It is often associated with other allergic conditions like asthma, and hay fever. |
As with any other skin condition, psoriasis is diagnosed through a combination of several diagnostic methods, such as:

There is no permanent cure for psoriasis. However, there are a variety of treatments available to effectively manage symptoms, reduce flare-ups, and improve quality of life. The best treatment plan depends on the severity of the condition, the type of psoriasis, and individual response to therapies. At Livingstone Dermatology, treatments can include:

Psoriasis is a chronic skin condition that stems from an overactive immune system, leading to inflammation, scaling, and discomfort. While it is not contagious, it can significantly impact one’s quality of life if left unmanaged.
It goes without saying that seeking medical advice early is key to managing psoriasis effectively. A dermatologist can provide a personalised treatment plan tailored to your condition, helping to control flare-ups, and improving skin health. Schedule a consultation with us today to take the first step towards healthier, and more comfortable skin.
Currently, there is no permanent cure for psoriasis. However, various treatments can effectively manage symptoms, and reduce flare-ups. With the right approach, including medications, lifestyle adjustments, and medical therapies, many people with psoriasis can achieve long-term remission, and maintain healthy skin.
No, psoriasis is not contagious. It is an autoimmune condition, meaning it results from an overactive immune system rather than an infection. You cannot catch psoriasis from another person through physical contact, sharing personal items or exposure to skin flakes.
Yes, scratching or injuring psoriasis plaques can break the skin barrier, making it vulnerable to bacterial infections. Signs of an infection include increased redness, warmth, swelling, pus, and pain in the affected area. If you develop a fever or notice worsening symptoms, seek medical attention promptly.
Psoriasis is more than just a skin condition as it can be linked to other health concerns. Some common complications include:
While psoriasis cannot be entirely prevented, certain lifestyle habits can help reduce flare-ups, and minimise symptoms. These include:
Psoriasis can impact daily life, but with proper management, many individuals continue to live full, active, and fulfilling lives. Seeking treatment, finding emotional support, and making lifestyle adjustments can significantly improve comfort, and confidence. If psoriasis is affecting your well-being, our dermatologist can help tailor a treatment plan to suit your needs.
Yes, some people experience periods where their psoriasis symptoms disappear completely — this is known as remission. Remission can last for weeks, months or even years, depending on individual triggers, and treatment effectiveness. However, psoriasis is a chronic condition, and flare-ups may return at any time. As such, consistent management, and professional guidance are key to keeping symptoms under control.
Diet alone does not cause or cure psoriasis, but certain foods may influence inflammation levels in the body. Some individuals find that reducing processed foods, excessive sugar, and alcohol while incorporating anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids can help manage symptoms. However, dietary triggers vary from person to person, so it is best to observe how your body responds.
At Livingstone Dermatology, we understand the impact psoriasis can have on your daily life. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Rosacea is a long-term skin condition that causes persistent redness, visible blood vessels, and sometimes acne-like bumps on the face. Although it is often mistaken for common skin sensitivities or acne, rosacea is a distinct dermatological concern that requires proper management.
While the exact number of people affected in Singapore is unknown, rosacea is more prevalent among adults aged 30 to 50 years old, particularly those with fair skin. If the condition is left untreated, symptoms can worsen over time, leading to increased discomfort, and self-consciousness.

Rosacea is an inflammatory skin disorder that primarily affects the central face, including the cheeks, nose, forehead, and chin. It often begins with episodes of flushing, where the skin temporarily turns red before returning to normal.
Over time, this redness can become persistent, and small, dilated blood vessels, known as telangiectasia, may appear. Some individuals also develop bumps or pimples that resemble acne, while others experience eye irritation, known as ocular rosacea.
Although rosacea is not contagious, it can significantly impact daily life by causing discomfort, and emotional distress.
Rosacea presents in different forms, each with unique characteristics, such as:
The exact cause of rosacea is not fully understood, but it is believed to result from a combination of genetic, environmental, and immune system factors. Some of the key triggers, and risk factors include:

While symptoms vary from person to person, some of the most common signs include:
Although rosacea primarily affects the face, it can affect different parts of the face, and body, including:
Diagnosing rosacea involves a thorough assessment of your skin, symptoms, and medical history. At Livingstone Dermatology a thorough assessment of your skin condition will be made, and you may expect the following:

When it comes to the effective management of Rosacea, the treatment plan generally focuses on reducing symptoms, preventing flare-ups, and improving skin health. While there is no cure, personalised treatments at Livingstone Dermatology can help control the condition and minimise discomfort.
In conclusion, rosacea is a long-term skin condition that causes redness, visible blood vessels, and sensitivity, often triggered by environmental, and lifestyle factors. Although it is not contagious, it can worsen over time if left untreated, leading to persistent discomfort and, in some cases, complications such as thickened skin or eye irritation.
Early intervention is key to keeping rosacea under control. Our skilled, and experienced dermatologist can diagnose your specific type of rosacea, and create a personalised treatment plan to manage symptoms, and prevent flare-ups. If you are experiencing ongoing redness, sensitivity or unexplained skin changes, do not wait for them to intensify. Schedule a consultation with us today, and take the first step towards clearer, healthier skin.
Is rosacea painful?
Is rosacea an autoimmune disease?
Rosacea is not classified as an autoimmune disease, but it does involve an abnormal immune response. The condition is thought to be linked to an overactive inflammatory reaction in the skin, as well as increased sensitivity to environmental factors, and microorganisms like Demodex mites.
While the exact cause is still being researched, rosacea shares some similarities with autoimmune, and inflammatory conditions in terms of immune system involvement.
How can I differentiate a rosacea rash from a lupus rash?
Both rosacea, and lupus can cause facial redness, but there are key differences:
Can rosacea be cured permanently?
Currently, there is no permanent cure for rosacea, but the condition can be effectively managed with proper treatment, and lifestyle adjustments. Many people with rosacea see significant improvements by following a personalised treatment plan that includes topical or oral medications, laser therapy, and trigger avoidance. Early diagnosis, and treatment can help prevent symptoms from worsening over time.
Can rosacea be prevented?
Since rosacea has a genetic and environmental component, it cannot always be entirely prevented. However, flare-ups can be minimised by identifying, and avoiding triggers such as excessive sun exposure, alcohol, spicy foods, and stress. Consistently using gentle skincare products, wearing daily sun protection, and following a dermatologist-recommended treatment plan can help keep rosacea symptoms under control.
If I have rosacea, does that mean I cannot wear makeup?
You can still wear makeup if you have rosacea, but it is important to choose products that are gentle, non-comedogenic, and free from irritating ingredients such as alcohol, fragrance, and harsh preservatives.
Additionally, look for mineral-based foundations, green-tinted primers to neutralise redness, and hydrating formulas that support skin health. On top of that, always remove makeup with a gentle, non-stripping cleanser to avoid aggravating your skin.
If you are unsure of the type of makeup or skincare products you should use, our dermatologist can recommend suitable makeup, and skincare options tailored to your skin’s needs.

A skin allergy is a condition in which the immune system reacts abnormally to a substance that is typically harmless, leading to inflammation and discomfort. When an allergic reaction occurs, the skin may develop redness, swelling, itching, rashes, or even blisters.
The way a skin allergy presents depends on the type of reaction, with some conditions causing immediate flare-ups, while others develop gradually over time. Below are some of the most common types of skin allergies:
Type | Description |
Contact Dermatitis | Occurs when the skin comes into direct contact with an allergen, leading to redness, itching, and irritation. Common triggers include nickel, fragrances, cosmetics, latex, and certain plants like poison ivy. |
Atopic Dermatitis (Eczema) | A chronic condition that causes dry, itchy, and inflamed skin. While often linked to genetics and environmental factors, allergens can worsen symptoms. It is common in children but may persist into adulthood. |
Urticaria (Hives) | Characterised by raised, red, and itchy welts that appear suddenly due to an allergic reaction to foods, medications, insect stings, or environmental triggers. Hives can be acute (lasting hours or days) or chronic (lasting for weeks or longer). |
Angioedema | A deeper form of swelling that affects the skin and mucous membranes, often occurring around the eyes, lips, hands, and feet. It may accompany hives and, in severe cases, can impact breathing, which may require immediate medical attention. |

A skin allergy occurs when the immune system mistakenly identifies a harmless substance as a threat and initiates a defensive response. This process begins when the skin encounters an allergen, prompting specialised immune cells called Langerhans cells to capture and present it to T-cells in the lymph nodes. If the immune system perceives the substance as harmful, it triggers the release of inflammatory chemicals, such as histamines and cytokines. These chemicals cause blood vessels to dilate, increasing blood flow to the affected area and leading to redness, swelling, and itching.
In some cases, the reaction occurs immediately, as seen in conditions like urticaria, while in others, such as allergic contact dermatitis, it may take hours or days to develop. Over time, repeated exposure to the allergen can intensify the immune response, making future reactions more severe. This hypersensitivity mechanism is what differentiates allergic reactions from simple irritant responses, which do not involve the immune system.
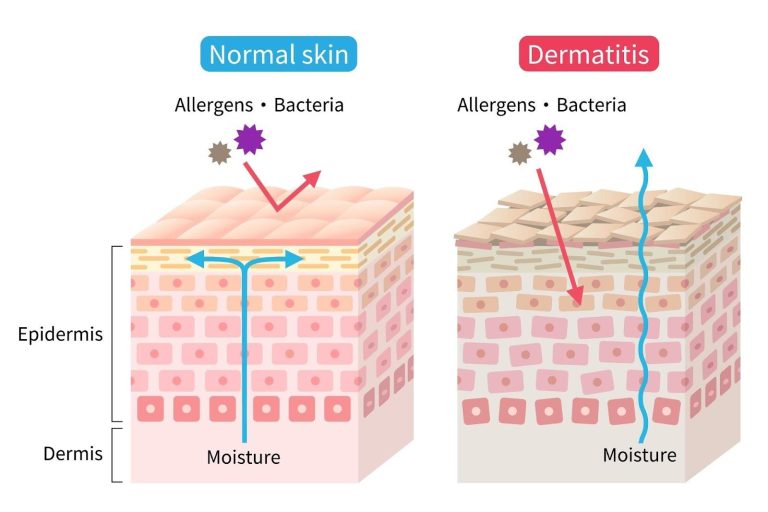
The symptoms of a skin allergy vary depending on the type of reaction and the severity of the immune response. Some symptoms appear immediately after exposure to an allergen, while others develop gradually over time. Common signs of a skin allergy include:
Symptoms can range from mild discomfort to more severe cases that require immediate medical attention, especially if swelling affects breathing or spreads extensively across the body.

Certain individuals are more susceptible to developing skin allergies due to a combination of genetic, environmental, and lifestyle factors. In Singapore, where high humidity and urban pollutants are common, some risk factors can further increase the likelihood of allergic skin reactions. These include:
Recognising these risk factors can help individuals take preventive measures to reduce their chances of experiencing allergic flare-ups.
Since allergic reactions can vary widely from person to person, we use varied diagnostic methods to pinpoint the exact cause of your symptoms. Our dermatologists assess your medical history, lifestyle factors, and environmental exposures before recommending specific tests to identify potential allergens.
Common diagnostic methods include:
Our dermatologists use a combination of medical therapies, skincare recommendations, and lifestyle adjustments to help you achieve long-term relief. Treatment options may include:
If you are experiencing persistent skin irritation, unexplained rashes, or allergic flare-ups, schedule a consultation with us for a detailed diagnosis and personalised treatment solutions.
While there is no definitive cure for skin allergies, effective management is possible through identifying and avoiding triggers, using appropriate medications, and following a proper skincare routine. Many individuals experience significant relief and may have prolonged periods without symptoms.
No, skin allergies are not contagious. They result from an individual’s immune response to specific allergens and cannot be transmitted from person to person.
Stress does not directly cause skin allergies, but it can exacerbate existing conditions. Managing stress through relaxation techniques and lifestyle changes may help reduce flare-ups.
Preventing flare-ups involves identifying and avoiding known allergens, maintaining a regular skincare routine with hypoallergenic products, and protecting your skin from environmental factors like extreme temperatures and pollutants.
Over-the-counter creams, such as hydrocortisone, can provide temporary relief for mild symptoms. However, it’s essential to consult a dermatologist for persistent or severe reactions to ensure appropriate treatment.
Certain foods may trigger or worsen skin allergies in susceptible individuals. Keeping a food diary and observing any correlations between diet and skin reactions can be helpful. Consulting a healthcare professional is recommended for personalised advice.
If you experience persistent, severe, or worsening symptoms, or if over-the-counter treatments do not provide relief, it’s advisable to consult a dermatologist. Professional evaluation can help identify specific allergens and develop an effective treatment plan.
At Livingstone Dermatology, we understand the impact skin allergies can have on your daily life. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of various types of skin cancers. Our experienced dermatologist offers expert care to ensure early detection, accurate diagnosis, and effective treatment for optimal outcomes.
Basal Cell Carcinoma (BCC): This is the most common form of skin cancer, typically appearing as a pearly or waxy bump, often with visible blood vessels.
Squamous Cell Carcinoma (SCC): SCC often appears as a red, scaly patch, a raised growth with a central depression, or a wart-like growth.
Melanoma: Melanoma is a less common but more aggressive form of skin cancer, often characterized by irregularly shaped moles with uneven coloring.
Actinic Keratosis (AK): Although not cancer itself, AKs are considered precancerous and can develop into SCC if left untreated.
Merkel Cell Carcinoma: This is a rare, aggressive form of skin cancer that usually appears as a painless, firm, and fast-growing nodule.
Early detection of skin cancer is crucial for successful treatment. Our dermatologists conduct thorough examinations, often supplemented by advanced imaging or biopsy techniques, to accurately diagnose and stage skin cancers.
At Livingstone Dermatology, we prioritize your skin health and overall well-being. Our experienced dermatologist is dedicated to providing expert care for individuals with skin cancers, guiding you through the diagnosis and treatment process with compassion and expertise.
Livingstone Dermatology specializes in the diagnosis and treatment of warts and verrucas. Our experienced dermatologists offer expert care to ensure effective removal and provide guidance on preventing recurrence.
Warts: Warts are non-cancerous growths caused by the human papillomavirus (HPV). They can appear anywhere on the body, often on the hands, feet, and face. Warts are typically small, rough, and may have a cauliflower-like appearance.
Verrucas (Plantar Warts): Verrucas are a type of wart that specifically develop on the soles of the feet. They may appear flat or have a rough, bumpy surface, often surrounded by hardened skin.
Warts and verrucas are highly contagious and can be contracted through direct or indirect contact with the virus. Common sources of infection include:
Our dermatologist provides guidance on preventive measures, such as avoiding direct contact with warts, keeping feet clean and dry, and wearing protective footwear in public areas.
At Livingstone Dermatology, we understand the discomfort and frustration that warts and verrucas can cause. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of urticaria, commonly known as hives. Our experienced dermatologists offer expert care to help you identify triggers and manage symptoms effectively.
Urticaria, more commonly known as hives, is a skin condition characterized by raised, itchy welts that can appear anywhere on the body. These welts often have defined borders and can vary in size and shape. Urticaria can be acute (lasting less than six weeks) or chronic (lasting longer than six weeks).
Urticaria can be triggered by a wide range of factors, including:
Our dermatologist conducts thorough evaluations to accurately diagnose urticaria and identify potential triggers. Treatment options may include:
While urticaria can be a chronic condition, with the right treatment and lifestyle modifications, it can be effectively managed. Our experienced dermatologists will work closely with you to develop a personalized treatment plan that addresses your specific needs and lifestyle.
At Livingstone Dermatology, we understand the discomfort and frustration that urticaria can cause. Our experienced dermatologist is dedicated to providing expert care and support, helping you find relief and regain control over your skin health.
Livingstone Dermatology specializes in the diagnosis and treatment of vitiligo, a skin condition characterized by the loss of natural skin color. Our experienced dermatologists offer expert care to help you understand and manage this condition effectively.
Vitiligo is a chronic skin condition that results in the loss of pigmentation, leading to the development of white patches on the skin. It occurs when the melanocytes, the cells responsible for producing melanin (skin pigment), are destroyed or stop functioning.
While the exact cause of vitiligo is not fully understood, it is believed to be related to a combination of genetic, autoimmune, and environmental factors. Certain triggers, such as stress, trauma, or illness, may exacerbate the condition.
Our dermatologist understands the impact vitiligo can have on self-esteem and body image. We provide support and guidance on living well with vitiligo, including skincare recommendations and advice on sun protection.
At Livingstone Dermatology, we are dedicated to providing expert care for individuals with vitiligo. Our experienced dermatologist works closely with you to develop a personalized treatment plan that addresses your specific needs and concerns.
Whether you’re dealing with a specific skin concern or seeking to enhance your natural beauty, Livingstone Dermatology is here to guide you on your journey to healthy, radiant skin.
Schedule an appointment today and experience the Livingstone standard of care in a welcoming, professional environment.