

Moles, sometimes coined “beauty marks”, are little spots on the skin that can either add charm or raise concern. Most adults have up to 40 moles on their body, and these growths are typically harmless and can be left alone.
However, in some cases, some moles can signal changes in our skin that shouldn’t be ignored. Whether you have always had them, or a new one appears, understanding moles and what they could potentially mean for your skin health is important.
Moles, or nevi (singular: nevus), are small, dark brown spots on the skin composed of melanocytes, or pigment-forming cells [1]. Moles can be present at birth or form throughout your life. Typically, moles form in parts of the body exposed to the sun.
The exact causes of moles are not clearly understood. However, certain features in people indicate their likelihood of developing moles, these include [2]:
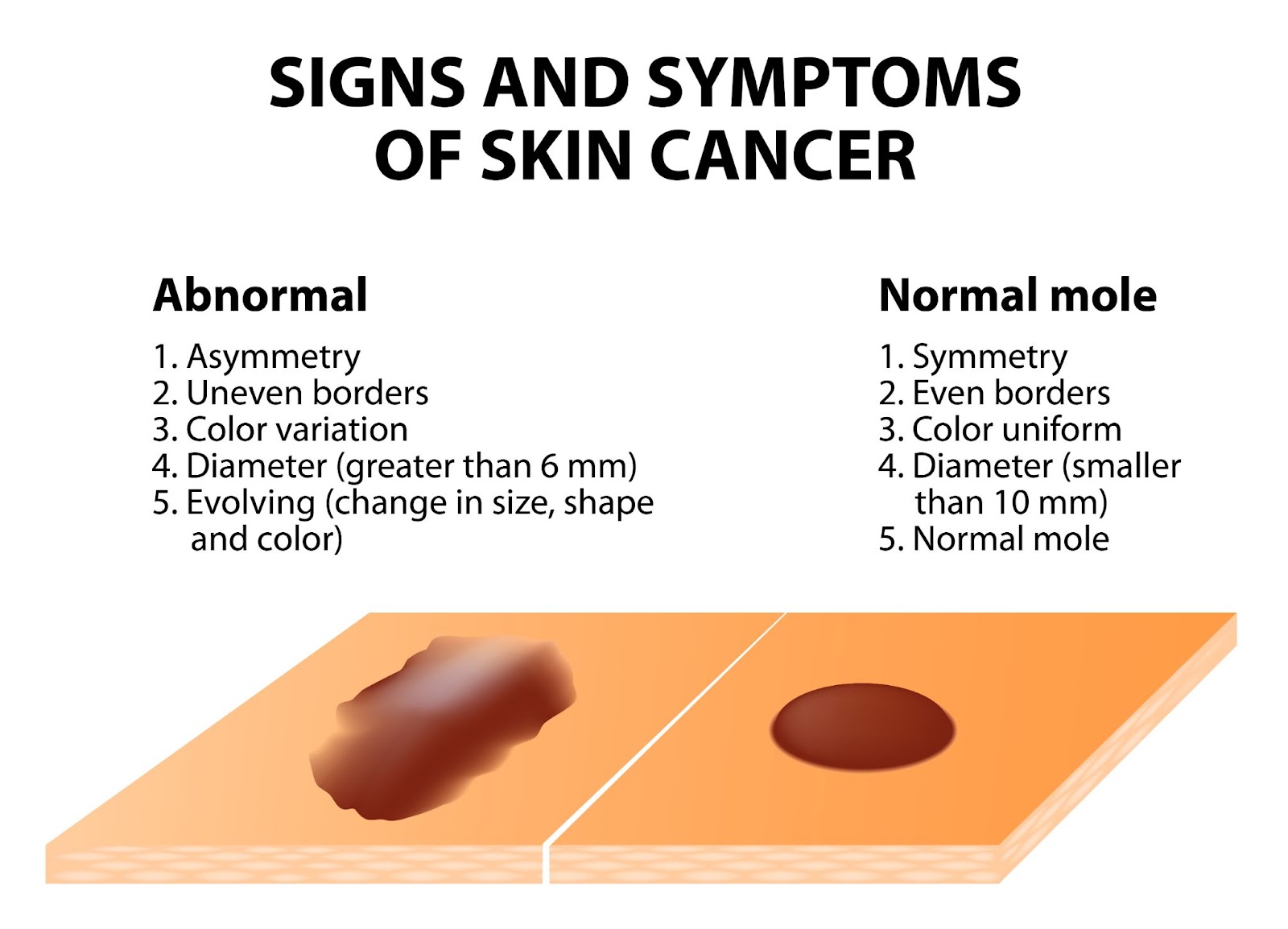
Most moles on our skin are harmless and can be left alone. However, moles can signify skin cancer. If you have a mole that you suspect is abnormal, a common guide to follow is the ABCDE guideline:
If you have moles with these characteristics, or notice these changes on a mole over a short period of time, it is highly recommended to get a dermatologist to assess the mole. Several helpful tips to take pictures and document changes of the mole include:
In addition to the features described in the ABCDE guideline, moles at risk of malignancy, or which are malignant may show the following characteristics:
In any case of doubt, it is always encouraged to visit a dermatologist for a thorough examination. Early detection of cancerous lesions allows treatment to be given early, preventing the spread of cancer cells. Once cancer has spread, it is more difficult to treat and manage, hence why early treatment can be life-saving.
Although moles are typically harmless and do not always need treatment or removal, many people opt to get them removed for the following reasons:
Typically, your dermatologist can recommend you to get a mole removed after assessment and diagnosis of the mole. A mole removal procedure can be done by the following treatments:
Before undergoing a mole removal procedure, it is important to get a proper assessment by a qualified dermatologist. Certain methods of removal, such as lasers, electrocautery, and cryotherapy, do not provide tissue samples for a biopsy. If your dermatologist suspects a mole for potential malignancy, they may recommend surgical excision, which can be followed by tissue biopsy for a proper diagnosis. Some removal methods are also at risk of mole recurrence, hence it is important to consult your dermatologist before undergoing any mole removal procedures.
After your removal procedure, your dermatologist will give you detailed instructions on how to care for the surgical wound. They may also ask you to come back for a follow-up visit to monitor your skin’s healing process, as well as to discuss biopsy results on the removed tissue if necessary.
Moles are common skin growths, are typically harmless, and do not necessarily require removal. However, there are cases where prompt assessment and removal are paramount in preventing skin cancer.
Regardless of the reason, it is always recommended to visit a dermatologist for a proper mole removal, as this limits the risk of infection, scarring, and mole recurrence. More importantly, if you experience a suspicious mole, book a consultation with us for a detailed assessment and personalised treatment plan.
Can I remove moles on my own?
Can I just have my mole removed at the spa by my therapist?
It is recommended to have your mole removed at a dermatologist’s office as it is medically supervised to ensure safe removal with sterile and precise techniques. More importantly, your mole can be properly assessed on whether it is benign or potentially cancerous — preventing risk of complications or missing a very serious condition.
When should I visit a doctor for mole removal?
Moles do not always need removal if they do not bother you, aesthetically or physically. However, if you notice abnormal changes of your mole, such as change in colour, size, and shape, or if it starts to itch, burn or feel painful, you should visit a dermatologist to get it assessed and diagnosed.
How can I prevent moles?
Some moles may not be preventable, especially if you are genetically predisposed to them. However, certain lifestyle habits can reduce mole formation, and also reduce the risk of melanoma development from moles:
Do moles get bigger with age?
Why do moles suddenly appear?
The exact reason why moles appear are not entirely understood, most moles appear in childhood or adolescence, some moles can also appear later in life which may be due to exposure to the sun. Some have also argued that hormonal changes, such as during pregnancy, causes new moles to appear. However, scientists have not found a clear relationship between pregnancy and new mole development.
How to stop moles from growing?
Benign moles are not likely to grow, and even if they did it will be very gradual over a period of several years, hence if you notice a mole growing rapidly over a short period of time, you should visit a dermatologist as it may be a sign of skin cancer. You can prevent the development of new moles by protecting your skin with sunscreen or protective clothing, as well as limiting your time outdoors.
Whether you’re dealing with a specific skin concern or seeking to enhance your natural beauty, Livingstone Dermatology is here to guide you on your journey to healthy, radiant skin.
Schedule an appointment today and experience the Livingstone standard of care in a welcoming, professional environment.