At Livingstone Dermatology, we understand that your skin is a reflection of your health and well-being. We are committed to the latest advancements in dermatological science, and dedicated to providing you with quality care.

A skin allergy is a condition in which the immune system reacts abnormally to a substance that is typically harmless, leading to inflammation and discomfort. When an allergic reaction occurs, the skin may develop redness, swelling, itching, rashes, or even blisters.
The way a skin allergy presents depends on the type of reaction, with some conditions causing immediate flare-ups, while others develop gradually over time. Below are some of the most common types of skin allergies:
| TYPE | DESCRIPTION |
| Contact Dermatitis | Occurs when the skin comes into direct contact with an allergen, leading to redness, itching, and irritation. Common triggers include nickel, fragrances, cosmetics, latex, and certain plants like poison ivy. |
| Atopic Dermatitis (Eczema) | A chronic condition that causes dry, itchy, and inflamed skin. While often linked to genetics and environmental factors, allergens can worsen symptoms. It is common in children but may persist in adulthood. |
| Urticaria (Hives) | Characterised by raised, red, and itchy welts that appear suddenly due to an allergic reaction to foods, medications, insect stings, or environmental triggers. Hives can be acute (lasting hours or days) or chronic (lasting for weeks or longer). |
| Angioedema | A deeper form of swelling that affects the skin and mucous membranes, often occurring around the eyes, lips, hands, and feet. It may accompany hives and, in severe cases, can impact breathing, which may require immediate medical attention. |

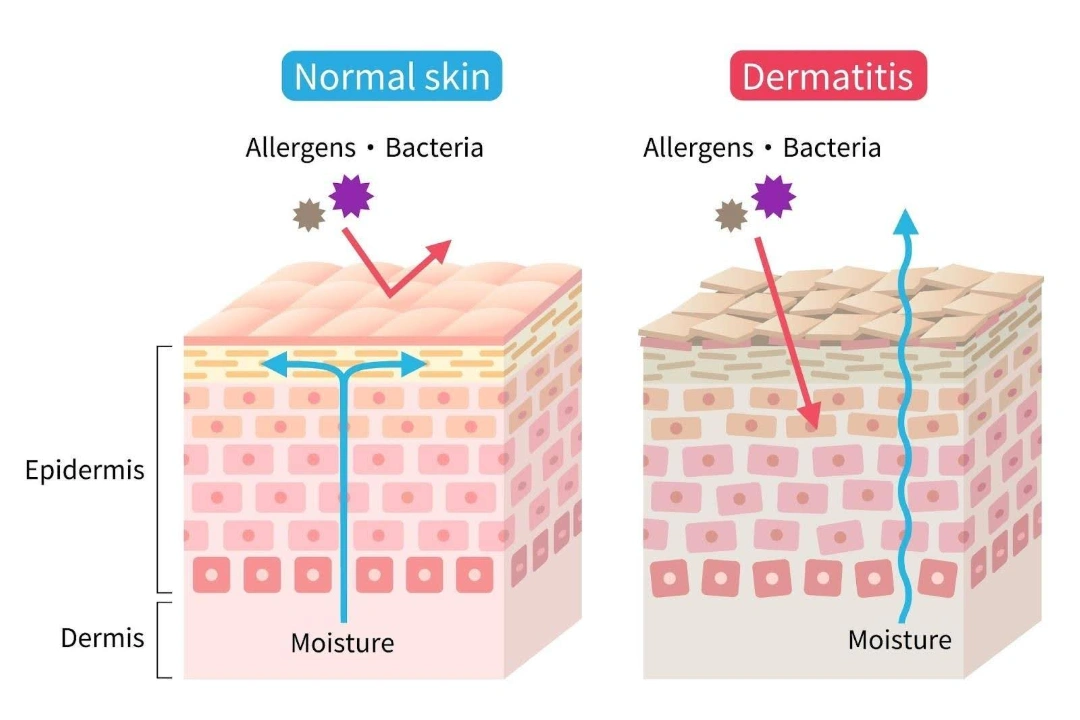
A skin allergy occurs when the immune system mistakenly identifies a harmless substance as a threat and initiates a defensive response. This process begins when the skin encounters an allergen, prompting specialised immune cells called Langerhans cells to capture and present it to T-cells in the lymph nodes. If the immune system perceives the substance as harmful, it triggers the release of inflammatory chemicals, such as histamines and cytokines. These chemicals cause blood vessels to dilate, increasing blood flow to the affected area and leading to redness, swelling, and itching.
In some cases, the reaction occurs immediately, as seen in conditions like urticaria, while in others, such as allergic contact dermatitis, it may take hours or days to develop. Over time, repeated exposure to the allergen can intensify the immune response, making future reactions more severe. This hypersensitivity mechanism is what differentiates allergic reactions from simple irritant responses, which do not involve the immune system.
The symptoms of skin allergy vary depending on the type of reaction and the severity of the immune response. Some symptoms appear immediately after exposure to an allergen, while others develop gradually over time. Common signs of skin allergy include:
Certain individuals are more susceptible to developing skin allergies due to a combination of genetic, environmental, and lifestyle factors. In Singapore, where high humidity and urban pollutants are common, some risk factors can further increase the likelihood of allergic skin reactions. These include:

Since allergic reactions can vary widely from person to person, dermatologists will use varied diagnostic methods to pinpoint the exact cause of your symptoms. Typically, they will assess your medical history, lifestyle factors, and environmental exposures before recommending specific tests to identify potential allergens.
Common diagnostic methods include:
Dermatologists will use a combination of medical therapies, skincare recommendations, and lifestyle adjustments to help you achieve long-term relief. As such, treatment options may include:
Skin allergy can greatly impact your quality of life, especially severe allergies. It can hinder you from performing basic day-to-day activities, and reduce your ability to work. The good news is that allergies are highly manageable. If you are experiencing persistent skin irritation, unexplained rashes, or allergic flare-ups, schedule a consultation with our dermatologists at Livingstone Dermatology for a detailed diagnosis and personalised treatment solutions.
Can skin allergies be cured?
While there is no definitive cure for skin allergies, effective management is possible through identifying and avoiding triggers, using appropriate medications, and following a proper skincare routine. Many individuals experience significant relief and may have prolonged periods without symptoms.
Are skin allergies contagious?
No, skin allergies are not contagious. They result from an individual’s immune response to specific allergens and cannot be transmitted from person to person.
Can stress cause skin allergies?
Stress does not directly cause skin allergies, but it can exacerbate existing conditions. Managing stress through relaxation techniques and lifestyle changes may help reduce flare-ups.
How can I prevent skin allergy flare-ups?
Preventing flare-ups involves identifying and avoiding known allergens, maintaining a regular skincare routine with hypoallergenic products, and protecting your skin from environmental factors like extreme temperatures and pollutants.
Is it safe to use over-the-counter creams for skin allergies?
Over-the-counter creams, such as hydrocortisone, can provide temporary relief for mild symptoms. However, it’s essential to consult a dermatologist for persistent or severe reactions to ensure appropriate treatment.
Can diet affect skin allergies?
Certain foods may trigger or worsen skin allergies in susceptible individuals. Keeping a food diary and observing any correlations between diet and skin reactions can be helpful. Consulting a healthcare professional is recommended for personalised advice.
When should I see a dermatologist for my skin allergy?
If you experience persistent, severe, or worsening symptoms, or if over-the-counter treatments do not provide relief, it’s advisable to consult a dermatologist. Professional evaluation can help identify specific allergens and develop an effective treatment plan.