At Livingstone Dermatology, we understand that your skin is a reflection of your health and well-being. We are committed to the latest advancements in dermatological science, and dedicated to providing you with quality care.

A nail biopsy is a medical procedure that involves taking a small tissue sample from specific parts of the nail for diagnostic purposes. This can be done by dermatologists to investigate certain abnormalities in the nail or its surrounding structures, such as deformities or lesions [1].
This is performed when there are abnormalities in the nail that cannot be diagnosed through a typical clinical exam or non-invasive tests.

No, a nail biopsy is usually recommended when other less invasive methods, such as a microscopy or culture, do not suffice in providing a diagnosis. It can also be performed if you experience progressive or worsening changes in your nails, as this could suggest a more serious underlying condition.
Nail biopsies are done to diagnose or rule out certain conditions of the nail or around the nail that cannot be diagnosed from other parts such as the skin, common conditions include:
Nail biopsies are performed when the indicated lesion is isolated in the nail, and cannot be diagnosed on other parts. Common conditions diagnosed via a nail biopsy include:
A nail biopsy can be recommended by your dermatologist if your nail condition is chronic and keeps returning. It is a helpful diagnostic approach to determine the best course of treatment for your condition. In certain cases, a nail biopsy diagnosis can lead to nail surgery, where your dermatologist will treat the condition.
Depending on the location and type of lesion, your dermatologist may choose to perform either of the following:
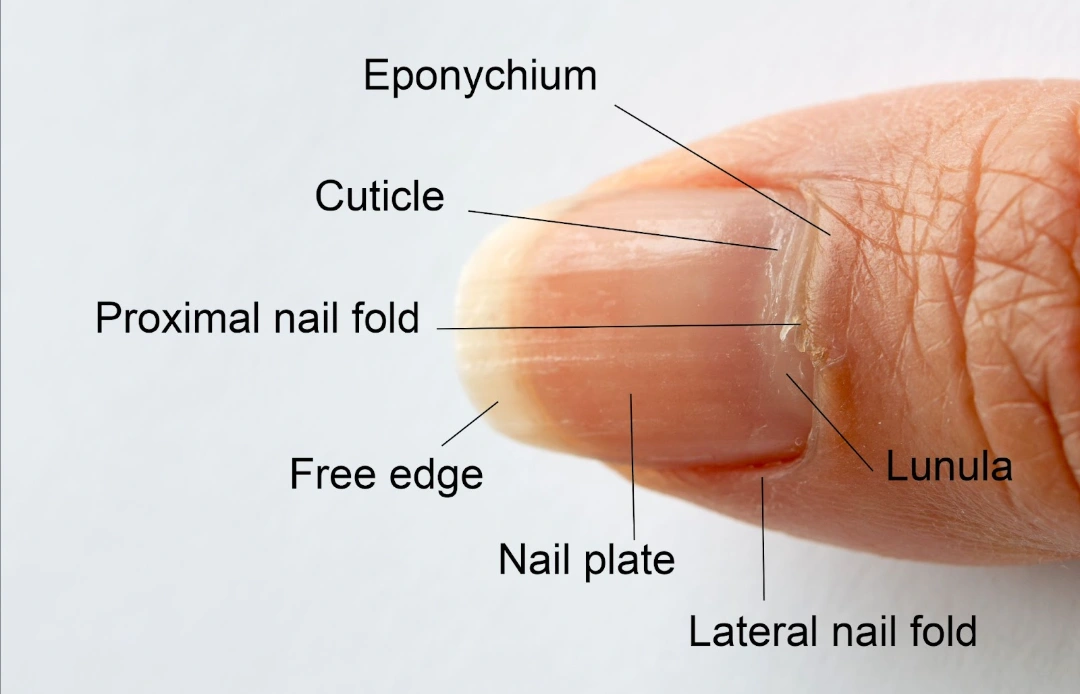
Aside from the location of the biopsy, the type of biopsy also differs in terms of procedure. Common nail biopsy procedures include [4]:
The type of nail biopsy you will need will depend on the dermatologist’s initial evaluation and assessment of your condition. The dermatologist will also go over risk assessment with you before performing a biopsy. Consult with our dermatologist if you have any doubts or concerns.
Are there any risks associated with nail biopsies?
Nail biopsies may involve invasive procedures, hence risks and side effects are present and should be well understood before undergoing a procedure. Risks associated vary with the type and location of procedure and technique. Less invasive techniques such as nail plate biopsies will come with lower risks than nail bed or nail matrix biopsies. Common complications of the procedure include [4]:
That said, these complications are rare, and having the nail biopsy procedure performed by a trained dermatologist significantly minimises these risks. It also helps to follow post-procedure care instructions provided by your doctor to further reduce any likelihood of complications.
What can I expect from a nail biopsy procedure?
The process of a nail biopsy typically goes as follows:
The time taken for the procedure depends on the type of biopsy, some procedures are relatively quick and can be completed in 15 minutes to half an hour.
Aftercare notes for your Nail Biopsy
Generally, after your procedure, your doctor will advise you on the following aftercare practices:
After this, you will have a follow-up session to monitor your healing and for your doctor to go through your biopsy results with you.
How long will it take my nail to heal after a biopsy?
Generally, how long it takes to heal from a nail biopsy largely depends on the extent of the procedure and the type of biopsy performed. Generally, here’s what to expect:
When should I visit a Dermatologist?
You should consult a dermatologist if you notice abnormal or concerning changes on your nails, such as:
Certain changes in the nail can be caused by injury, chemotherapy, or stress. If these are unlikely to have occurred recently, seeking professional medical help is highly recommended.
Just like hair and skin, nails can reflect our health and well-being. When something seems out of the ordinary or starts to cause discomfort, a consultation to a dermatologist can be helpful in identifying and managing your concerns.
Here at Livingstone Dermatology, we are dedicated to providing personalised, expert care for every aspect of your skin health, including your nails. If you’re experiencing persistent nail concerns or unusual changes, schedule a consultation with us today for a comprehensive diagnosis and treatment plan tailored to your needs.
Does a nail biopsy hurt?
Local anaesthesia is usually administered to reduce pain and discomfort during the procedure. It is generally well-tolerated, and you may only experience some pressure, but no sharp pain.
Will the nail grow back normally after a nail biopsy?
Yes, a nail biopsy that does not damage the nail matrix should allow the nail to grow back normally. However, there are still risks of regrowth defects.
How long does the procedure take?
Depending on the site of biopsy, the procedure may take anywhere from 15 minutes to several hours. For example, biopsy of the nail matrix or nail bed that requires anaesthesia and specialised tools and techniques will take longer than biopsy of the nail plate.
What can I not do after a nail biopsy?
The dermatologist will advise on post-operative care after your nail biopsy, this may vary on a case by case basis. General care of the digit may include changing bandages, keeping it dry, and elevating the digit for the first 48 hours after surgery. Strenuous and risky activities should also be avoided to reduce risks of injury and pain.
Whether you’re dealing with a specific skin concern or seeking to enhance your natural beauty, Livingstone Dermatology is here to guide you on your journey to healthy, radiant skin.
Schedule an appointment today and experience the Livingstone standard of care in a welcoming, professional environment.