
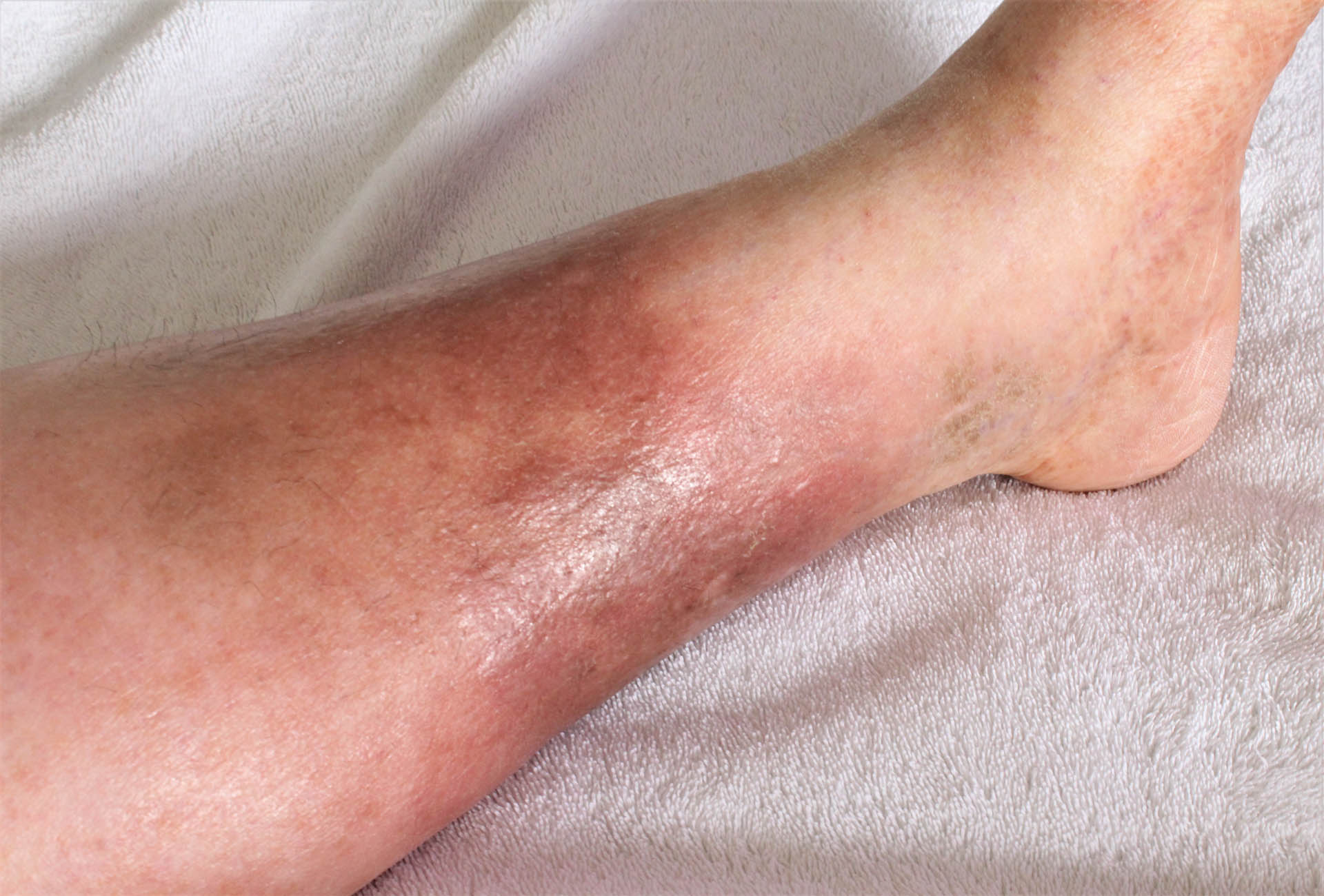
Skin infections develop when bacteria, viruses, or fungi enter the skin and trigger inflammation, discomfort, or visible changes. In many cases, these infections are mild and respond well to treatment, but even small or early signs should not be dismissed. Seeking timely medical care helps ease symptoms more quickly, lowers the chance of complications, and prevents the infection from spreading to others.
Certain circumstances can make skin infections more likely. Hot and humid environments provide ideal conditions for microbes to thrive. Breaks in the skin, such as cuts, grazes, or areas affected by existing conditions, give germs an opportunity to enter. Crowded or shared spaces, including schools, sports facilities, or childcare centres, also increase the risk of passing infections from one person to another.

The infections can appear on almost any part of the body, though some areas are more frequently affected depending on the cause and individual risk factors. Common sites include:
The skin is the body’s largest organ and serves as a vital barrier against harmful microbes. Normally, it protects us effectively from bacteria, viruses, and fungi. Infections can occur when these pathogens find a way in, often through hair follicles or breaks in the skin caused by cuts, scrapes, burns, insect bites, or other injuries.
Several factors can increase the likelihood of a skin infection, including:

The types of infections can be grouped based on the type of germ causing them. Each type brings its own set of signs, symptoms, and quirks, but all share one thing in common: they happen when harmful microorganisms find a way past our skin’s natural barrier.
Some of the common skin infections include:
Bacterial infections
Viral infections
Fungal infections
Parasitic infections
While the symptoms of skin infections vary with the infectious agent that causes the lesion, some of the common signs are:


Who is at risk of developing Skin Infections?
Anyone can develop an infection, but certain individuals are more vulnerable due to factors that weaken the body’s natural defences. Most of the time, the immune system can fend off minor infections, yet specific conditions or circumstances can make it easier for pathogens to take hold.
Some of the groups that are more susceptible to contracting skin infections include:
How are Skin Infections diagnosed in Singapore?
Once a skin infection is suspected, our dermatologist will usually begin with an in-office assessment. The exact approach depends on the type of infection, its severity, and your symptoms. Common methods include:
Depending on the suspected pathogen, our dermatologist may also order more specific tests, such as:
What are the treatment options available for Skin Infections in Singapore?
After a diagnosis is made, the treatment focuses on targeting the specific microbe responsible for the infection. The approach depends on the type, severity, and location of the infection. But it generally involves:
At Livingstone Dermatology, we prioritise treating skin infections promptly and effectively. Proper treatment not only clears the infection but also reduces the risk of complications and prevents it from spreading to others. Early medical care is key to a safe and speedy recovery.
Protect your skin and overall health by consulting a qualified dermatologist if you notice unusual rashes, redness, or sores. Our team provides accurate diagnoses and personalised treatment plans tailored to your needs. So, call us today to schedule an appointment and safeguard your health.
Are skin infections contagious?
Many skin infections can spread through direct contact with an infected area, contaminated objects, or shared personal items. Practising good hygiene and avoiding sharing towels, clothing, or grooming tools can help prevent transmission.
Can skin infections come back after treatment?
Yes, some infections may recur, especially if the underlying cause is not addressed. These include poor hygiene, friction in skin folds, or a weakened immune system. Following our dermatologist’s advice and preventive measures can reduce the risk of recurrence.
How long does it take for a skin infection to heal?
Healing time varies depending on the type of infection and its severity. Mild infections may improve within a few days of treatment, while deeper or more serious infections can take weeks and may require ongoing monitoring.
Can home remedies help with skin infections?
Some mild infections may benefit from supportive home care, such as keeping the area clean and dry. However, most infections require medical evaluation and targeted treatment to prevent complications or spread. Avoid self-medicating with antibiotics or antifungals without a dermatologist’s guidance.
How can I prevent skin infections in the future?
Preventive measures include:
For those with underlying conditions like diabetes or eczema, extra care is needed to protect the skin barrier.
Are there any long-term complications from untreated skin infections?
Untreated skin infections can worsen over time and sometimes lead to serious health issues. Potential complications include:
Whether you’re dealing with a specific skin concern or seeking to enhance your natural beauty, Livingstone Dermatology is here to guide you on your journey to healthy, radiant skin.
Schedule an appointment today and experience the Livingstone standard of care in a welcoming, professional environment.